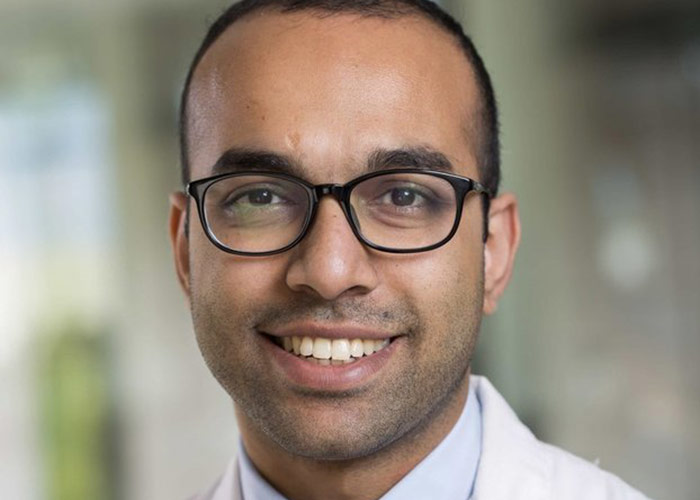
We had fun on this in-studio podcast with Dan Matlock, geriatrician and palliative care clinician researcher at the University of Colorado, and frequent guest and host on GeriPal. We most recently talked with Dan about Left Ventricular Assist Devices and Destination Therapy.
Today we talked with Dan about Implantable Cardiac Defibrillators (ICD) and Cardiac Resynchronization Therapy (CRT) – everything a geriatrician or palliative care clinician should know. Dan and his team have developed a number of terrific decision aids around ICD implantation (see patientdecisionaid.org), and have seen uptake and use of these decision aids skyrocket following CMS’s mandate requiring an shared decision making interaction prior to ICD implantation.
Enjoy!
-@AlexSmithMD
Eric: Welcome to the GeriPal podcast. This is Eric Widera.
Alex: This is Alex Smith.
Eric: And Alex, we have-
Alex: Wait, wait, wait…
Eric: Wait. There is somebody else in the room.
Ken: Hi.
Eric: Who is that person?
Ken: I’m Ken Covinsky.
Alex: Oh, yes.
Ken: Thanks for inviting me back.
Alex: It’s only like our 100th and something episode. I probably should have this down by now.
Eric: Okay. And we have another special guest. We have Dan Matlock, who’s been a frequent host, guest, on this podcast in the past. Dan Matlock is a geriatrician, a palliative care doc, and researcher at the University of Colorado. Welcome to the GeriPal podcast once again.
Dan: Thank you for having me.
Eric: Great that you’re here in studio. Well, we’re going to be-
Alex: Otherwise known as Eric’s office.
Eric: We’re going to be talking about what geriatricians, what palliative care clinicians and providers should know about ICDs and CRTs. And if you don’t know what those mean, we’ll get to that too. But before we do, we always start off with a song request. Do you have a song request for Alex?
Dan: Yeah, let’s do the Sound Of Silence, by Simon and Garfunkel.
Alex: All right. We do a little bit of harmony too, little bit.
Dan: We’ll try.
Alex: [singing 00:01:49]
Dan: [singing 00:01:49]
Ken: Bravo.
Alex: Yeah, we had a little bit of harmony.
Eric: Nailed it.
Alex: Nailed it. Yeah, nailed it.
Alex: It was perfect in every way.
Eric: Why did you choose that song?
Dan: It’s just one of my favorite songs. Anytime it comes on the radio it has this like deep darkness. I saw Paul Simon sing it live, and he basically played it with a guitar and the light just on him. And he basically talked it like a poem and it was just haunting.
Eric: Who did it better?
Dan: He did.
Alex: When the ICD fires, it’s silent? No?
Eric: I think you’re going to hear a lot of yelling when the ICD fires.
Alex: That’s probably true.
Eric: So Dan, this is not the first time you’ve been on our podcast. We had you on before, talking about LVADs and decision making around LVADs. Highly encourage all of our listeners to go to that. And you also came out recently, in 2019, with a Jags article titled ‘Implantable Cardio Defibrillators and Cardiac Resynchronization Therapy in older adults with heart failure.’ We’ll have a link to that on our GeriPal podcast, but we want to run with that idea and thinking about what do we need to know about ICDs and CRTs in the populations that we care for?
Alex: Maybe it’d be helpful, for me at least, to start off with what is an ICD and what is CRT? And what’s the difference? And are they the same?
Dan: So ICD stands for implantable cardioverter defibrillator. It’s like a little piece of a hotel soap size thing, just like a pacemaker, sits onto your skin, has some wires to your heart and it senses dangerous rhythms. And if it sees one, it shocks it, just like those external defibrillators like you see on TV. CRT is different. It stands for cardiac resynchronization therapy, sometimes also called biventricular pacing. It’s basically a synonym. About 40% of people with differentiators have this type of pacing.
Dan: And what that does is, it has a third wire, it has a wire to the right atrium, a wire to the right ventricle, but a third wire that goes through this fragile vein called the coronary sinus, to the left ventricle. So it has three wires, and what it does is, it gets the right and left side of the heart to beat together and gives you a little more blood flow, a little more cardiac output and the people feel better. And there’s pretty good data that CRT will make you feel better, it gives you a little more blood flow, if you have the sort of indications for it, a widened QRS interval, not to get too detailed, but it will make you feel better. And whereas the defibrillator doesn’t make you feel better, just senses that dangerous rhythm.
Alex: And can you have a CRT device that is not a defibrillator or all…
Dan: You can.
Alex: You can?
Dan: You can have… And that’s a really good question because you can choose just to have the CRT for the quality of life benefits and then not have the defibrillator because you might say, “Dying a sudden death isn’t the worst thing that could happen, I want to feel better. But if I’m going to die a sudden death, let me go.” In Europe, they do a good job doing just CRTPs or CRT pacing without the defibrillator. In the United States, basically if you get a CRT, it’s kind of a knee jerk, you’d get it with the defibrillator.
Alex: So combo package? It’s a combo package.
Dan: They’re two really separate decisions that get highly conflated.
Eric: All right, so can I take a step back before… Let’s focus on ICDs for a second. What is the indication for ICD, let’s say in heart failure?
Dan: So in heart failure, this is for people who’ve never had a cardiac arrest, that’s a whole separate thing. If you had a cardiac arrest, then you have a whole different list of indications. But if you’ve never had a cardiac arrest, then it’s just people who have heart failure of a certain condition. So an ejection fraction less than 35% and class two or three heart failure symptoms. Those are the people that are eligible for a defibrillator.
Eric: And I’m guessing, in those studies that they did, given this is a condition of old age often, that they’ve probably enrolled a lot of older adults in these studies that showed benefit.
Dan: No.
Eric: What?
Dan: No. That was the setup. I feel it. [laughing]
Alex: Well, luckily when we go to the CRT discussion, you’re going to tell us otherwise, but let’s focus on ICD.
Dan: Yeah. The average age in the trials was 61. Average age of people with heart failures, 74.
Eric: That’s a big difference.
Alex: That is a big difference.
Eric: So I’m trying to get a handle on what this thing is. So when you say ICD, so defibrillator, I kind of have this vision of when you watch, like ER on TV, they take out this thing and they put paddles on you.
Dan: Yeah.
Ken: So is it like, you have somebody puts paddles inside of you? What exactly, what does it look like to a patient to have one of these things? Do you know that you have it in you most of the time or is it?
Dan: Well, you know you have it in, but it’s like a little pacemaker, so it just sits under the skin and sticks out a little bit. And then those wires in the heart will sense the rhythm and they will deliver a shock just like those external pads. Now, they do it with a little less energy, so those external pads, to use an electric term, are about 150 to 300 jewels of electricity, whereas the internal ones are about 10 jewels of electricity. So it’s less, but patients still feel it if they’re awake. If they haven’t passed out from the bad rhythm, they’ll feel it. And they describe it as, like getting kicked in the chest by a mule or… I had a patient who got shocked by his defibrillator and fell backwards into the towel rack and had a big old gouge in his back with stitches from getting shocked by his defibrillator.
Eric: I’m going to go back to the Jags article and I’m going to present a case to you, and I’d just love you to… How do you think about whether or not this person should get an ICD? So the case was, in the Jags article, an 81 year old male, New York Heart Association, class two to three functional status, has ischemic cardiomyopathy, EF 25%, frailty, osteoporosis, diabetes, CKD. And you’re considering primary prevention for ICD. Should we just do it?
Ken: What do you mean by primary prevention? What’s that?
Eric: So he hasn’t had a life threatening arrhythmia, right?
Dan: Right. That’s, that’s the primary prevention. The secondary prevention are those people who’ve had the life threatening arrhythmias.
Ken: So when you’re talking about primary prevention, is you’re talking about primary prevention of death, right?
Dan: Of sudden cardiac death.
Ken: Okay. Most people don’t want that. That seems pretty good to me.
Dan: Yeah. No, it’s interesting. If you ask people, do you want to prevent sudden death? They say, yes. You ask people, do you want to die in your sleep? They say, yes. So now you have a decision, and so I think that’s how you take this guy and you start talking to him about really, “What are your goals? What are your hopes? What are you hoping for out of the rest of your life?” This is assuming he’s not so frail that there may not be a benefit, but let’s say he’s not so frail and he may actually have a benefit. I think that it’s an interesting question in geriatrics. There’s a couple… One of the things that, actually a lot of articles out of San Francisco. “Well, these people are too old and sick for these things to be beneficial, we shouldn’t do them.” That’s one question, but then the other question is what if they’re old and sick, but they still might get some sort of ‘benefit’ from this device? I think that’s a much harder question and then that gets into this decision making where you really need to have a conversation, and if his goal is to live as long as possible and he doesn’t mind getting shocked, and he understands what he’s getting into and he’s not worried about a procedure, a defibrillator may be the right thing for him.
Alex: Is there anything that could help doctors who are struggling to have these conversations with patients, that just don’t know where to begin?
Dan: Well, that’s a low hanging curve ball. I appreciate it.
Ken: Does anyone work on that problem, Dan?
Dan: Alex knows some of my research. Yeah, we’ve done a lot of work on decision aids for patients making decisions around defibrillators.
Alex: And where would people find these decision aids?
Dan: www.patientdecisionaid.org. They’re available free, there is a video and a PDF version.
Eric: People don’t say the “www” anymore.
Dan: Oh, they don’t?
Eric: Well, I don’t know. I do. [laughing]
Alex: I say the whole thing. “Https:\”. [laughing] I actually was perusing through your site today and looked at the ICD guide, and one of the graphs that I noticed was… Because what happens, you get these ICDs, it’s not like the heart failure disappears, so you still will have periods of ups and downs and functional decline from the heart failure over time. And the one graph shows, if you have the ICD, you see this continued functional decline until death, but the group that didn’t get the ICD, you see this functional decline and then you have that sudden death event. And I thought that was a really interesting graphic, just to see it, “Oh yeah, it doesn’t fix everything.” It’s this issue, like you were talking about before, of what happens when we’re trying to prevent that sudden death in somebody who has this progressive life limiting illness.
Dan: Yeah. When I present a cardiology audiences, those are my favorite graphs to show because they… In the cardiac literature, mortality is this lumped together end point and those graphs’ sort of peel apart and show the flavors of mortality, and then you show the ICD is only treating this one flavor. And by the way, for some people that one flavor is not a bad flavor. Right now, I have three daughters, I would probably get a defibrillator if I had heart failure. But there’s a time in my life when, maybe my wife has died, my kids are a little sick of me, I get short of breath walking to the mailbox, and dropping dead of sudden death isn’t the worst thing that could happen.
Dan: Certainly those of us who take care of older adults in a senior’s clinic, hear that from patients all the time. And that’s where that preference sensitivity comes apart. And that actually, when speaking to cardiologists, they understand that, it’s just that their literature doesn’t present it that way. But this is just treating sudden death. And then once you see that, and then once you see sudden death as a little bit of a preference sensitive thing, then all of a sudden how you treat that guy becomes a function of a conversation about him and his goals and his values.
Eric: And the other thing I liked about it, you had a graph of a hundred people, I think it was a 100 people, showing how many people actually may benefit from this in the entire population. Do you remember that graph?
Dan: Oh yeah.
Eric: Do you want to describe it a little bit for me?
Dan: Yeah. So that’s from a big trial in 2005 now, in the new England Journal, but showed, out of a 100 people, seven people would have their life prolonged by a defibrillator, 29 out of a hundred would still die. So compared to what we do in primary care with cholesterol and hypertension, that’s a pretty big benefit.
Eric: And that’s over a course of five years?
Dan: Five years. So that’s one and a half percent a year, but it’s not a huge number, but it’s a number. And so yeah, I think it’s a beneficial therapy and there’s a couple papers that have tried to do observational research in older adults and in the right patients, there are some older adults who might get the benefit in prevention of sudden death from a defibrillator.
Eric: And do we think, like an older adults, do we think we’re going to see more benefit, less benefit, about the same benefit as that 2005?
Dan: I don’t think we know for sure. And I’ve looked at this a bunch. I think probably a little less because you get different competing mortalities. If you’re a young person with heart failure, sudden death is probably the most likely way to go for some populations. As you get older, you get competing mortality. But the absolute rate of sudden death, just because you’re more likely to die, the absolute rate goes up. So you still get a pretty similar absolute risk reduction, at least in a couple of the studies that have looked at it.
Eric: Can I just… This is probably a stupid question never thought about before. What does sudden death look like in somebody with the progressive pump failure? How is that defined in somebody with a progressive, disease like heart failure?
Dan: If you die of progressive pump failure, let’s say you’re having increasing heart failure, your heart’s getting weaker, then you go into a bad rhythm and just die. That’s sudden.
Eric: That’s sudden. Okay. Any bad rhythm?
Dan: Yeah. Versus your heart just gets weaker and weaker and you’re in an ICU and your fingers get cold. That’s the pump failure, kind of.
Eric: But everybody eventually dies.
Dan: No. [said jokingly]
Eric: Having seen plenty of people die on tele, you always see that, fatal arrhythmia at the very end.
Dan: Not all of them are shockable rhythms.
Eric: Okay.
Dan: A lot of people… Nate Goldstein actually, he’s a palliative care geriatrician at Mount Sinai. Tried to look at this in one of his trials, not everybody dies of an arrhythmic death, like ventricular tachycardia or ventricular fibrillation. Some people just die of PEA, pulseless electrical activity, and that’s not shockable.
Ken: Okay. So it sounds like, the question you asked, Eric, is pretty important, that sounds like sudden death can be a lot of different things. So that, on the one hand, there’s the sudden death of somebody who was living a good quality of life, maybe in spite of some heart failure and their life was going to be interrupted by a rhythm disturbance, which could be corrected, and then they returned back to their normal life, which could have considerable time left. But then there could be people who are so sick and so debilitated that they almost could be in hospice, but while their death is going to be sudden, you kind of knew it was coming. And you could kind of see this in an extreme case where they’re actively dying and they have a defibrillator that doesn’t let them die, but they’re not really living, they’re living but not. So how do we console patients about these different…
Dan: Yeah.
Ken: Would a typical cardiologist talk to a patient about these kind of differences in these different ways a defibrillator could work? Because it sounds like some are pretty good and some are pretty bad.
Dan: Yeah. No, I think you’re also asking a very good question. I think it gets into where geriatricians and palliative care physicians can really intervene with defibrillators as people get sicker. It may have made a lot of sense when this person was 70 or 75, to put the defibrillator in, but now they’re 80 or 85 or have metastatic cancer. If they’re dying of something else, it probably is a good idea to turn it off, and you can turn off the defibrillator function, you don’t have to do new surgery, you can just turn it off externally with a computer and a little wand that has some magnets in it.
Dan: But that discussion needs to be had. And I don’t think cardiologists are doing a lot of that, and I do think they should do more of that. And I think, since they see these patients frequently, they should own that a little bit and tell them. And I think they want to do the right thing, it’s just hard to know when somebody is there, as we all know, it’s really hard to know. But I think that’s where we as geriatricians and palliative care people, can really help.
Eric: Are there guidelines around, if your prognosis is less than a year, then you’re less likely to benefit from an ICD or cardiac resynchronization therapy?
Dan: Yeah, there are guidelines about turning off defibrillators. I don’t remember how specific they are.
Alex: You need to do a prognosis.
Eric: Well, how about for placing them? So for placing a defibrillator, is there some sort of… You said earlier about how they might be too sick or frail to benefit, but is there no limit? There’s no guideline around?
Alex: I thought there was, less than a year. It’s part of that age and comorbidities in the strict, saying no to ICD, but you should have consideration if prognosis is less than a year. Does that sound familiar?
Dan: It does, although I don’t want to misquote the guidelines on a podcast. But there is something there, it’s just, the exact words are not coming to me.
Alex: But it should be a consideration?
Dan: Yeah, it should be a consideration.
Eric: And let’s say, because I think it’s really important for people who run hospices or palliative care services, to screen for things like ICDs, because if your patient has it, you’re transitioning to focus on comfort, making sure that they’re not getting kicked by a mule is really important.
Dan: Oh yeah.
Eric: Any suggestions on, if we’re creating this process, what is the best way to turn it off? Is it calling the cardiologist that did it? Is it calling the device manufacturer, or what?
Alex: Get a refrigerator magnet or what?
Dan: So refrigerator magnets, big magnets, do work. You put the magnet… If you’re in a hospice and somebody’s just laying there, getting shocked over and over, you can put magnets on them and that will deactivate the defibrillator. But you don’t want to get there, you want to plan for that ahead of time, which is what you’re asking, Eric, and I think you can call the cardiologist, usually it’s a device nurse. If you know what company, if it’s a Medtronic or whatever company put in the device, you can call the representatives from that company and they can come turn it off. They’ll probably feel, they want the doctor’s orders who put it in. I’ve had that experience actually, in a hospice, where we called them and they didn’t want to do it until they talked to the electrophysiologist, so that was just painful, but we made it happen. But there’s ways to do it, but it is getting on the phone to somebody who has that computer and machine to turn it off.
Alex: Great.
Eric: How about CRT? What’s the indication for CRT? Or primary prevention?
Dan: So CRT is, again, it’s for that quality of life and it’s for people with advanced heart failure who have a widened QRS. So they have the right and left side of their hearts are beating at different times, so you can see that on an EKG where the area, the QRS interval they call it, gets wide. And it’s those patients, very similar to defibrillators, but then you put the CRT in and then those patients feel better. I think that’s a very different decision.
Ken: So this basically fixes the failing electric system in your heart, to bring the two chambers pumping together?
Dan: Right.
Ken: So I noticed, when you were talking about the defibrillator, you talked about living longer, but now you’re talking about feeling better. That sounds really good.
Dan: Yeah.
Ken: Who wouldn’t want that?
Dan: Yeah. And I actually think it is a very different decision. I can see a lot of older adults who might say, “I wouldn’t mind having that thing that helps me feel better, but I don’t want that thing that’s going to shock me.” But that requires a discussion and I think they are different decisions in that way. And like I said, in Europe they have that discussion. In the United States, we just put the defibrillator in and don’t really talk about it.
Ken: Is there any money behind that? Do you get paid more if you do both?
Dan: I don’t think the CRT with the defibrillator pays that much more, than just the CRT. Although, I don’t know the numbers. I think most of the costs are there. So I don’t think it’s about money, I think it’s about docs believing the defibrillators are things patients should have.
Eric: So the CRT makes people feel better, from the studies. We heard a little bit about ICD studies not enrolling older adults, but I’m guessing the CRT studies, they came out a little later, so they must have a much higher average age and…
Dan: Kind of 80s and 90s, yeah.
Eric: Like the people that were putting these things in.
Dan: Yeah. No, I don’t know the numbers like I knew the other one, but they are not, they’re not focusing on older adults. It’s still in the 60s for the averages.
Eric: Although, I was interested to read in your Jags article, that quality of life seem to be better for older patients. Cardiac resynchronization therapy.
Dan: This is fascinating.
Dan: And there’s a couple of models on this and a lot of things we see, that the benefits of whatever said therapy, get less as you get older. With CRT, the models seem to go the opposite direction, where you seem to get a little more benefit as you get older and sicker, so you don’t want to leave these things that might help your patient feel better. You don’t want to withhold those from them because they might be too expensive. And I don’t know if that’s… Maybe as a society we need to have that discussion, but as a doctor taking care of a patient, it might be a good thing to do, if they’re willing to take the risks of the procedure. Now, the risks of CRT, the procedural risks are a little higher.
Eric: In older adults?
Dan: In everybody. But almost certainly-
Eric: Higher than ICD?
Dan: Yeah.
Dan: Because that that third wire, going down that little vein, that vein has really thin walls and you can just puncture right through it, and then you’re bleeding into the chest and you need… It doesn’t happen that often, but it can happen and it’s different, it’s a different complication. You don’t want to dissect the coronary sinus vessel that’s draining the blood from the heart.
Eric: That sounds bad.
Dan: It’s a bad thing to do.
Eric: Bad thing to do.
Ken: Actually, as I’m a proud member of the less is more society, but is this one of these things where I could be neglecting something in my older patient, just because I’m assuming it’s not indicated because they’re all old?
Dan: Yeah, I think that’s one of the points in that paper, and the other authors on that paper were cardiologists or electrophysiologists. But I think that’s one of the point, is that, just because you’re old, these things might be helpful. And at the same time, you get to a point with everybody where more procedures is not helpful, and you might still not do it.
Eric: And we talked about deactivation of ICDs. It sounds like you can’t… A CRTD, is that doing that right?
Dan: It’s hard to do.
Eric: So you’ve got the defibrillator part, you can deactivate the defibrillator. Should you ever deactivate the CRT component, because I guess it makes it feel better, right?
Dan: Yeah. It’s same thing with pacemakers at the end of life, which comes up a lot, and people ask, “Should we turn off the pacemaker?” And you often don’t because the pacemaker is helping people feel better. There’s a rare instance where, say, somebody’s in an intensive care unit and they’re having the ventilator taken out, and they may want to then turn off the pacemaker too. But for the most part, when I work with patients, if they say, “I just want to turn everything off.” I really make sure they understand that that might mean they don’t feel as good.
Eric: Yeah. Well, it’s interesting. We’ve had a couple of people who’ve, I think, rightfully decided that they wanted to stop the pacemaker and a lot of pushback of nobody actually wanting to deactivate it. That’s not something that I can deactivate, you actually need the EP person, the Medtronic folks to actually come out and do that, and a whole lot of… Like Katie Butler actually wrote a book about that too.
Dan: Yeah.
Alex: With her father, yeah.
Dan: And I think there are situations where it’s right, but a lot of times I think people are thinking, “I just want to stop all these things and let me go.” Okay, we can do that. But if we stop that, you might not go and you might just sit there and not feel well with a pulse of 35, and then you’re just getting short of breath, but you’re still alive. And is that really what you mean? And I just want to make sure people really know what they’re getting into when they say, “I want to stop the pacemaker.”
Eric: Yeah.
Ken: That’s a pretty novel concept, to try and understand what your patient wants.
Dan: It’s a good thing to do.
Eric: Wow.
Ken: But that’s kind of fascinating, because what you’re implying is, we have all these vast technologies, these really expensive technologies, but you still, even with these expensive technologies, you still have to know how to talk to a patient.
Dan: Yeah.
Ken: That’s pretty clever.
Eric: What if the re-numeration for that conversation was equal to the… Okay, half of the re-numeration for doing the procedure itself to place the device?
Dan: I think that would create a lot of good conversations.
Eric: What if there was a site you can go to that, let’s say, had decision aids that could help me with these conversations?
Ken: I wonder if anyone’s developed those?
Eric: Have you thought about that?
Dan: Someone ought to. Patientdecisionaid.org. You can do a www if you want.
Alex: On the internet.
Eric: And you have decision aids on that for both ICDs, CRTs, CRTDs, and whether or not to replace a ICD or CRT, right?
Dan: Yeah. And that’s another thing, after five to seven, or maybe 10 years, depending, the battery runs out and people think, “Oh, I need a battery replaced.” But that’s actually an opportune time to talk to them about, do they still want this? Does it still meet their goals? Because now they have seven to 10 years of data, living with it, and maybe they were shocked a couple of times and it prevented lethal arrhythmia, and they don’t have post traumatic stress disorder and they’re really happy with it, and you replace it. Or maybe now, it’s never touched them, now they have dementia and a lot of comorbidities, and maybe this is no longer consistent.
Eric: It seems like that’s opportune time, as you suggest. Is there a choosing wisely statement about this? The time of battery replacement is an optimal time to readdress… Or, goals of care and continuation of ICD or CRT should be discussed at every battery replacement among older adults.
Dan: I feel like there should be, I don’t know if there is one. That would be a great one actually. That’s a good choosing wisely.
Eric: Yeah. Maybe we can convince some people, I don’t know if we can, but maybe Rheta Redbird can convince some people. We’ll talk to her about that at dinner tonight.
Dan: Yes, sounds good.
Eric: Are there any other interesting policy issues around this or?
Dan: There’s really interesting policy issue around this. So Medicare, last year, mandated shared decision making for anybody getting a defibrillator and they mandated it with use of a decision aid, and this is the third time Medicare has done this mandating shared decision making. They did it with lung cancer screening and they did it with the left atrial appendage occlusion for patients with a-fib, and then they did it for defibrillators. And from where I stand, it’s both good and bad. For my clinical trial, it’s basically completely contaminated my control group.
Eric: No. Oh, no.
Dan: But the trial is a combined effectiveness implementation, so it’s really enhanced the implementation piece as we study now. Now that people have to do it, there’s this impetus to figure out how do we do it easier, how do we do it better, which has created all kinds of opportunities for me from a research perspective, and a design perspective. How can the design… Now that you’re willing to use this, because you have to, what can we design to really make it helpful and how do we create that? Use a tool to create the conversation.
Dan: I just had a nice conversation with Ken Covinsky about, how do these tools talk about emotion? And I think ideally, these tools support a conversation, but at the end of the day, it’s a doc, a clinician and a patient having an emotional conversation about preventing sudden death or whatever it is. And so, can these tools enhance that somehow? And with this mandate, which the cardiology community, I would think, very comfortably say that they’re not a fan of, I don’t think I’m putting words in their mouth, but it does, it’s creating all kinds of fun discussions. Like I got invited to Heart Rhythm Society to speak, which I hadn’t been to before.
Eric: Oh. They’re the ones who, they work very closely with industry and are well funded by industry, if I recall?
Dan: Yeah. It was here in San Francisco, and the little industry expo room was like nothing I’d ever seen.
Eric: Interesting, yeah.
Ken: Yeah. So Medicare, when you say they mandate this, they mandate that electrophysiologist wants to put in a defibrillator, so what we’ve been calling an ICD. So in order for them to get paid for that, the patient has to be given a decision aid. So this means that they’re going to spend like an hour talking with you this or does this just mean they hand you a piece of paper and say here’s your decision aid, and now we can… Does Medicare do anything to make sure this happens well?
Dan: Yeah. No, no. It could be done anyway and it could be done as they hand it to you and then check the box. And I think that’s what’s happening a lot, is people are checking the box. But interestingly, before the mandate, everything I learned from the docs, said I don’t want anything that takes more time in clinic. So we made a video, we made a tool, that people could watch on their own and the implementation model was, “Watch this before you see the doc.” At our local VA, they mail the video out to every patient. The guy I work with there is an electrophysiologist, he’s in the video, he’s really bought in. Mails it to them and he says the discussions are better when they see it. But now, with the mandate, the community’s wanting some shorter tool that they can use in the clinic.
Dan: So in case a patient shows up, they don’t know why they’re there. Now they have to do shared decision making. They want something that supports the conversation. But I think that’s a design question. Do you design something for people to use in the encounter? Which needs to be a different design than something used outside? I think there’s a lot of room for innovation in designing decision aids, to really fit contexts.
Eric: Now, I’ve been known to be somewhat nihilistic about decision aids. Like, “Great, you get a lot of research money to develop these things.” But does anyone actually use them in real world practice? And I sort of felt like, “No, they don’t.” But now it’s being mandated, people are using them to some extent, may not be high quality. Is this the biggest use of decision aids and this sort of example our case of decision aids in real world practice? People actually using them?
Dan: I don’t know if it’s the biggest. It’s big, our website, we’re getting three or 400 hits a day, and we get people contact us, asking if we can mail them some of the tools or can they purchase some, or is it okay for them to print, is it okay for them to put their hospital logo on there? So it’s definitely getting used. I think it’s getting used as a checkbox. The ELVAD tool we spoke about previously, we have a followup study where we’re trying to disseminate that nationally. And there’s about a 180 accredited ELVAD programs, and right now a 111 of them are using the decision aid.
Eric: Oh wow. Great.
Alex: That’s great. Wow.
Eric: Can I ask you a question? In the mandate, is there any discussion about what should be in these decision aids? I noticed in yours, you also talk about, which a lot of people don’t know, “Can I turn this thing off once it’s in?” And I think that’s a big question that’s never really addressed when they’re put in, or at least not often addressed. And I noticed you did. Is there a mandate of what needs to be discussed?
Dan: No, there’s no mandate. There’s a few suggestions in the mandate of what should be discussed, but there’s no mandate. It just says you have to use a ‘evidence-based decision aid in the CMS lodge.’ But even that’s interpreted as like, “Oh, it’s based on a trial, so it’s evidence based or it’s an effective decision aid, it’s evidence-based. That’s even debatable.” So CMS has not given a lot of guidance on that, on what they want. There are some guidelines around what a decision aid should have, but whether you turn it off or not isn’t necessarily in the guidelines, except that it emerged in our developmental work as an important piece. And that sentence in there was about an hour with our focus group of how do we talk about this in a way that’s not too scary, but make sure people are informed? And the option of turning it off is one of our key knowledge items. We did one survey before that, 60% of people didn’t even know you could turn it off.
Eric: Actually, that sounds right. The good face of validity to that.
Dan: A study I would love to do, but never going to really be able to design is, if you know you can turn it off, then maybe if it does shock you, maybe you’re less likely to have anxiety or post traumatic stress disorder, because you had some agency and you chose to have it, rather than it’s just happening to you and you have no control. We need a huge sample size to test that hypothesis, so I don’t think I’ll be able to. But it’d be a really cool one to test.
Eric: Well, I think… Really appreciate having you in the office. Really want to encourage people to also listen to the ELVAD podcast. We also use… Excuse the telephone. We also have a podcast with Nate Goldstein about heart failure, and discussing a little bit about his work with ICDs as well. So we’ll have that link on, also, our GeriPal podcast webpage. And with that, maybe before we end, we can hear a little bit more harmony.
Alex: Feel free to join in. And the words of the profits are written on the subway walls and tenement halls.
Eric: And that’s for all our listeners, right?
Alex: No, that’s for you and Ken.
Eric: Oh, no. Okay.
Alex: Because Dan and I will be singing this one.
Alex: [singing 00:37:02]
Dan: [singing 00:37:10]
Eric: And with that, I’d like to thank everybody for joining us today.
Alex: Thank you, Dan.
Eric: Dan, huge thank you for joining us.
Alex: Thank you guys. Thank you Ken.
Eric: Thank you Ken. And to all of our listeners in the audience for joining us.
Alex: Thank you Archstone Foundation. Thank you, bye.
Eric: Goodbye everyone.