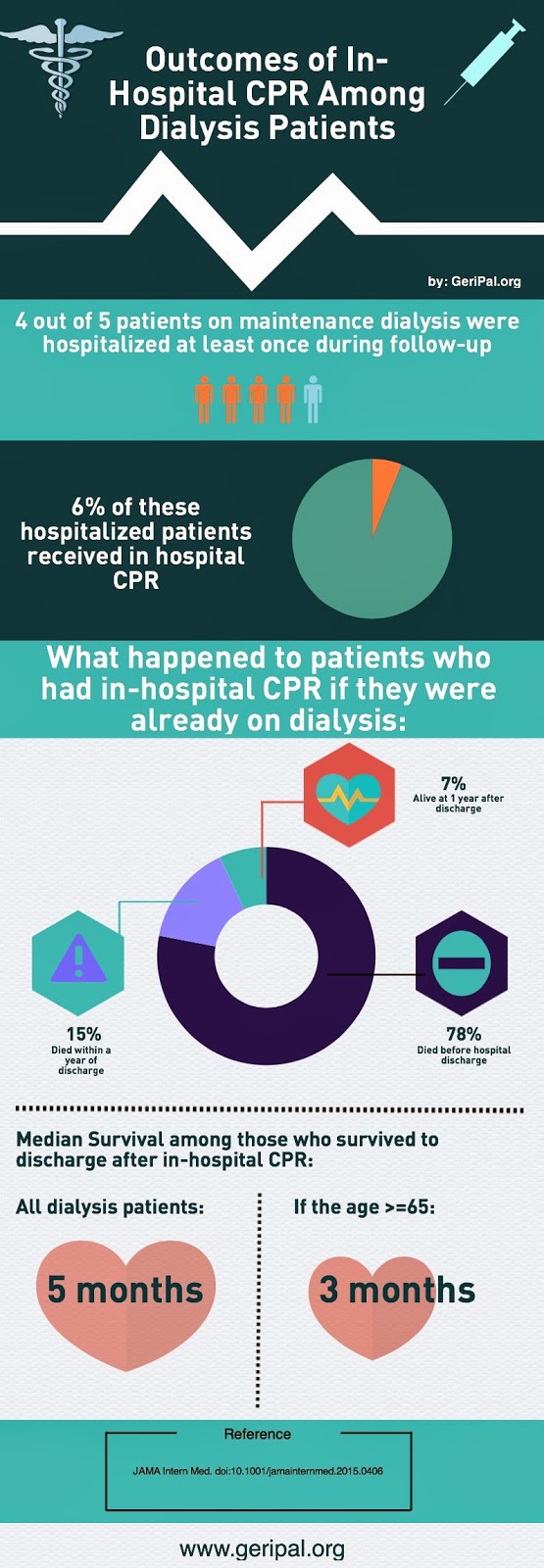
We’ve talked a lot about the prognosis after receiving in-hospital CPR in this blog (here, here, and here to name a few). In a recent issue of JAMA Internal Medicine, Susan Wong and colleagues looked at what happens to individuals on maintenance dialysis when they receive in-hospital cardiopulmonary resuscitation (CPR). The results are summarized in the infographic above, and discussed in a little more detail below.
The Study
The authors used data from the US Renal Data System (USRDS) registry that enrolls patients after the onset of end stage renal disease, identifying all patients 18 years or older without a prior kidney transplant who initiated maintenance dialysis from January 1, 2000, through December 31, 2010. Importantly, to be included in this study, these patients needed to be on dialysis for at least 90 days (thereby exluding the sickest of the sick). By linking Medicare claims, they determined who in this registry was hospitalized and who got in-hospital CPR (although they excluded ER CPR).
Outcomes of interest included incidence of in-hospital CPR, proportion of patients
surviving to hospital discharge after their first inhospital CPR event, and post-discharge survival. Among those who died in the hospital, they also measured the proportion who received CPR during their terminal hospitalization.
What did they find?
Most of the key findings are in the infographic, but I’ll just highlight a few here:
- The vast majority of individuals on maintenance dialysis were hospitalized at least once during the follow-up period (81% of the cohort)
- Of these individuals who were hospitalized, 6% underwent at least one episode of CPR while hospitalized with a trend toward higher rates of CPR in more recent years.
- The proportion of CPR
recipients who survived to discharge has increased in from 2000 to 2011 (15.2% to 28%) but there was no
substantial change in duration of post-discharge survival. - The median survival fromthe time
of discharge was 5.0 months among those who survived to discharge.
The Take Home
The results of this study are in line with other studies that suggest less people die in the hospital, but that doesn’t mean that their long-term prognosis is any better. In particular, Joan Teno’s work shows that despite a decline in hospital deaths and an increase in hospice use, end of life for Medicare decedents increasingly includes ICU stays, short hospice stays, and multiple health care transitions. This is particularly true to the dialysis population who undergo CPR. We are better able to get them out of the hospital alive, but their survival after hospital discharge really has not improved, making them otherwise prognostically eligible for hospice.
by: Eric Widera (@ewidera)
Note: for more on the geriatric and palliative care needs of those with end-stage renal disease see these posts: