Many clinical decisions in older persons are dependent on life expectancy. For example, as life expectancy declines, cancer screening is likely to do more harm than good. Also, persons who have limited life expectancy may want to plan, discuss their values, and consider palliative care approaches of care in addition to care focused on living as long as possible.
But can one actually predict life expectancy accurately in an individual patient? In an oustanding review of prognostic indices to predict life expectancy in older persons just published in JAMA, Dr. Lindsey Yourman suggests the glass may be more then half empty. Dr. Yourman is an internal medicine resident at Scripps Mercy Hospital in San Diego. Other authors include Alex Smith (senior author), Sei Lee, and Eric Widera of UCSF and Mara Schonberg of Beth Israel Hospital.
So what are the problems with prognostic indices? Well first, at least when applied to an individuals, they are of limited accuracy. For example, lets say you apply a prognostic index to 2 patients. If the index were perfect, it would always assign a lower life expectancy to the patient who dies first. However, Yourman found the best indices identified the patient who dies first no more than 85% of the time. Many indices identify the right patient less than 70% of the time. When you consider that flipping a coin will be correct 50% of the time, this does not sound so great.
But it is even worse than that. The accuracy of prognostic indices is often tested under ideal and controlled conditions. When you see a research report of a prognostic index, you see how well it did in a group of patients specified by the researchers. But how accurate will the index be in your patient? Invariably, the answer is less accurate. This is because your patients are never quite the same as the patients in the research study. Further, you will probably measure the risk elements in a somewhat different way than the researchers.
The answer to this seems simple enough. If we want to know the accuracy of the prognostic index, it should be tested by a new group of investigators in completely new patients. But as Yourman reports, this is almost never done.
So, does this mean we should do away with prognostic indices? No. It just means we should use them intelligently. Prognostic indices are ultimately not that different from any other clinical tool or diagnostic test. Just like you should never look at a test result in isolation, you should never look at a prognostic estimate in isolation. You think about the extent to which it is likely to apply to the patient right in front of you. You think about whether there are characteristics of your patient that were not considered in the prognostic index. And you use it as an additional tool in decision making–integrating the information with knowledge about the patient’s clinical circumstances, and their values and care preferences.
As an additional source of information, prognostic indices can be quite valuable, if used to supplement clinical judgement. But clinicians who use them in isolation, to supplant clinical judgement are probably better served by avoiding prognostic indices.
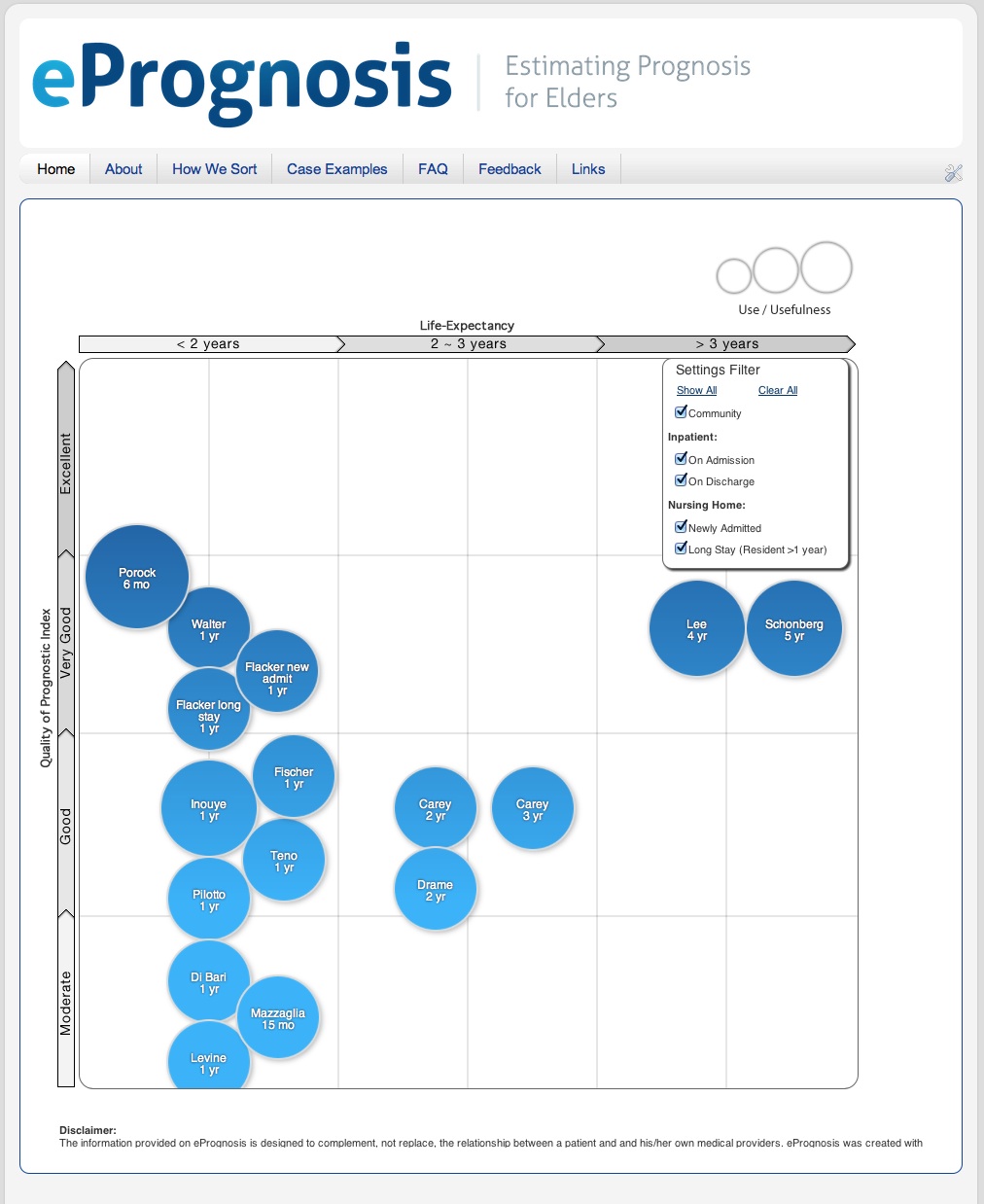
Clinicians (and patients too) now have easy access to these prognostic indices. The authors of the JAMA article have developed a website, ePrognosis, that has converted all the indices reviewed in the article to easy calculators. It is a great tool, that will improve access to prognostic information. But perhaps the danger of ePrognosis is that it is too easy. In a matter of minutes, you can input a few elements of patient data and the calculator will spit out a probability of survival.
Using ePrognosis intelligently will take much more work. Whether that number is actually accurate for your patient, and how you should apply it to their care is as much medical art as science.
by: Ken Covinsky