This is the first in a two part series on Geriatrics, Palliative Care, and Chronic Kidney Disease.
One of our most popular GeriPal posts ever is titled, “Dying without Dialysis.” That post discusses an article on the symptomatic experience of persons who decided not initiate dialysis in the setting of advanced kidney disease.
This is obviously a compelling topic, given the high prevalence of kidney disease among older adults.
Medicare policy that poses tremendous barriers to continuing dialysis while enrolling in hospice. This sets up an either-or dichotomy that leads to low rates of hospice use, and among those who use hospice, lengths of stay that are frequently 3 days or fewer.
This week, Eric and I talked with Melissa Wachterman, a physician researcher from the Dana Farber Cancer Institute and Harvard Medical School. Melissa used a national dataset of people receiving hemodialysis linked to Medicare claims for older adults who died. She found:
- 20% used hospice (compared to 48% hospice use among all Medicare decedents)
- Of those who used hospice, 42% used hospice for 3 days or fewer.
This is a complex issue, with not only the structural policy barriers, but also major communication issues, including lack of prognostic discussion and honesty.
Links:
- Melissa Wachterman’s article on Dialysis and Hospice, published in JAMA Internal Medicine
- Melissa’s article on Dialysis patient and physician perspectives on prognosis, also in JAMA Internal Medicine
-by Alex Smith, @AlexSmithMD
Eric: Welcome to the Geripal podcast. This is Eric Widera.
Alex: This is Alex Smith.
Eric: And Alex, who is our guest today?
Alex: Today we have Melissa Wachterman, who is at the Dana-Farber Cancer Institute and VA Boston and the Brigham Women’s Hospital, where she is a palliative medicine clinician and researcher. Welcome to the Geripal podcast, Melissa.
Melissa: Great. Thanks for inviting me.
Eric: We start off with every podcast with a song request. Do you have a song request for Alex?
Melissa: Yeah, “Running Down a Dream”, by the recently deceased Tom Petty.
Alex: And you saw him in concert a little bit before he died, isn’t that right?
Melissa: I did. He was rockin’ out. I’m not quite sure. I mean I guess I did hear what happened but we won’t go into that. But, yeah. No, it was like end of July he was totally rockin’ out and then saw the obituary like a month later.
Alex: It was very sudden. Yeah. Here we go. [Singing]
Melissa: Wow. Wow. Channeling the great. Impressive.
Alex: Tom Petty’s fun.
Eric: So we’re going to be talking about your article about the association between hospice length of stay, healthcare utilization and Medicare costs at the end of life among patients receiving maintenance hemodialysis that was published in JAMA IM this last month. Maybe before we go into the details of the article, can you tell us how you got interested in this subject?
Melissa: I’ve been studying patients with end stage renal disease for a while now and one of the things that’s been sort of loud and clear in this population is that they are sort of really sick and they really, their quality of life near the end of life isn’t great, so I feel like there’s a lot of room for us to improve things. Another thing that we found is that they don’t use hospice a lot. I think that what wasn’t as clear was, okay, so those that actually do get to hospice, sort of what are the differences? What are things like for them? The main driver question that I was really interested in is how long are they in hospice?
Alex: Yeah. Do you have any personal clinical experiences with this issue that you could, in an anonymized fashion, relate to our audience, so that it’s HIPAA compliant?
Melissa: Yeah. Sure. Sure. Yeah. I … Another piece that I have been studying is decision making about dialysis initiation. I, sort of pulling it into a patient I actually on wearing the hat of a medicine attending … I do palliative care attending but also medicine attending and I was wearing the medicine attending hat and we had a patient who was a relatively young, functional guy, a veteran, who actually had advanced liver disease. Really advanced liver disease, to the point that he had hepatorenal syndrome from his end stage liver disease, but it was pretty sudden onset.
As I say, he was a functional guy up until that point, or relatively so, and it became clear that time was short, clearly. He had hepatorenal syndrome but that dialysis probably would buy him a little more time at the point in which we were meeting him in the hospital. He lived at a distance and really, really wanted to get closer to home. He was six or seven hours from home. So then the question came up, “Okay, so are we going to do dialysis or not?” It was one of these things just thinking about decision making when you’re wearing the attending hat compared to the palliative care attending hat. It can feel kind of different in terms of basically I felt like in goals and values and the palliative care doctors were doing more in depth analysis that doing dialysis probably did make sense for him with the goal of getting home. So then it became, ok how are we going to help support this guy who has a very poor prognosis? To me, it was just a no brainer. Send this guy with hospice, potentially he may need inpatient hospice but he’ll be so much closer to home. But then there hits the policy barrier that as long as he’s going to get dialysis he can’t get hospice.
Alex: Yeah.
Melissa: And so it actually was, while I was writing this paper was when it came up. Yeah.
Eric: So, maybe a little bit of background, just because this gets into a complicated, thorny issue around dialysis and hospice. What is, what can be done in hospice with dialysis?
Melissa: Right. If your hospice diagnosis is end stage renal disease, you cannot get hospice until you stop dialysis.
Eric: And that’s because, not because Medicare says you can’t do it, but just that Medicare won’t fund or pay for dialysis anymore.
Melissa: Right.
Eric: So that’s the hospice’s responsibility and hospices would go broke if they were paying for dialysis in their patients. Is that right?
Melissa: Yes. That is basically right. I think that there are some people that just do you qualify for this diagnosis of end stage renal disease? Even just a qualifying for hospice under that Medicare diagnosis. I think it can be a little fudgy in terms of, because there’s always two issues. Do you qualify for, do you have a hospice diagnosis, and then exactly what will Medicare cover?
Eric: Do you mean that from a prognostic standpoint, like figuring out somebody who’s on maintenance dialysis, are they hospice eligible with a prognosis of less than six months?
Melissa: Well, right. That’s where I think the data is very clear, that there are a lot of patients on dialysis who have a prognosis of less than six months. Hands down, no question. That’s where I feel that there’s a little bit of a bias that people, and I think this gets at some other issues around just people on dialysis, doctors, like, “Oh, well, this is dialysis. That takes care of my kidneys. I’m good to go.” I think that some other work that we’ve done in the past that patients often have a much more optimistic picture of prognosis than they actually do. I do think that it’s not, “Well, as long as you’re on dialysis, you’re going to live more than six months”. Nothing is perfect, but there are prognostic models out there like we can do as good a job as we can in many non-cancer conditions with prognostication. It’s not just, “Well, we can’t find these people”. We can identify the people who are at high risk for dying in six months.
Alex: So, Melissa, in that case that you described, is it possible that a hospice qualifying diagnosis might have been the patient’s liver disease and liver failure?
Melissa: Yes. This does come up and this is where I feel like … right. The way we talked about it being when it’s your hospice diagnosis you can’t get dialysis and Medicare won’t pay for dialysis and hospice together. But, yes, if you qualify under another diagnosis, for example, right, he had end stage liver disease. That’s actually a really good point.
Eric: I actually think in that case, because the dialysis is related to hepatorenal syndrome, which is related to his liver disease he would not qualify.
Alex: Interesting.
Eric: He would actually have, and I won’t say he won’t qualify. He would have to …
Melissa: Pay. The hospice would have to pay for it.
Eric: Yeah. Hospice would have to for it-
Melissa: Yeah, exactly
Eric: … because it’s related to the terminal illness.
Melissa: That’s right.
Alex: It’s related. So if your patient had developed, had pre-existing … If a patient, this would be a completely different patient, had pre-existing need for dialysis due to poorly controlled diabetes and then developed a cancer that was fatal, then that situation, that patient could qualify for hospice under the cancer diagnosis while still receiving dialysis, paid for separately by Medicare, for the long standing end stage renal disease?
Melissa: Yes. That is exactly right. That’s exactly right and it’s the example I often use is the metastatic cancer one. It feels very arbitrary that in that case, exactly, you could continue to get the dialysis because it’s not related to your hospice diagnosis. I do think, and Eric, I think that’s great the way the hepatorenal syndrome one really susses out the issues between issue versus a qualification issue and you’re exactly right. The patient would qualify, but the hospice would bear the brunt of paying for the dialysis, which you sort of opened with. Hospices just can’t stomach that cost with the amount that Medicare pays for per diem hospice.
Alex: So tell us what you did in this study, like succinctly understanding that many of our listeners are clinicians and not researchers.
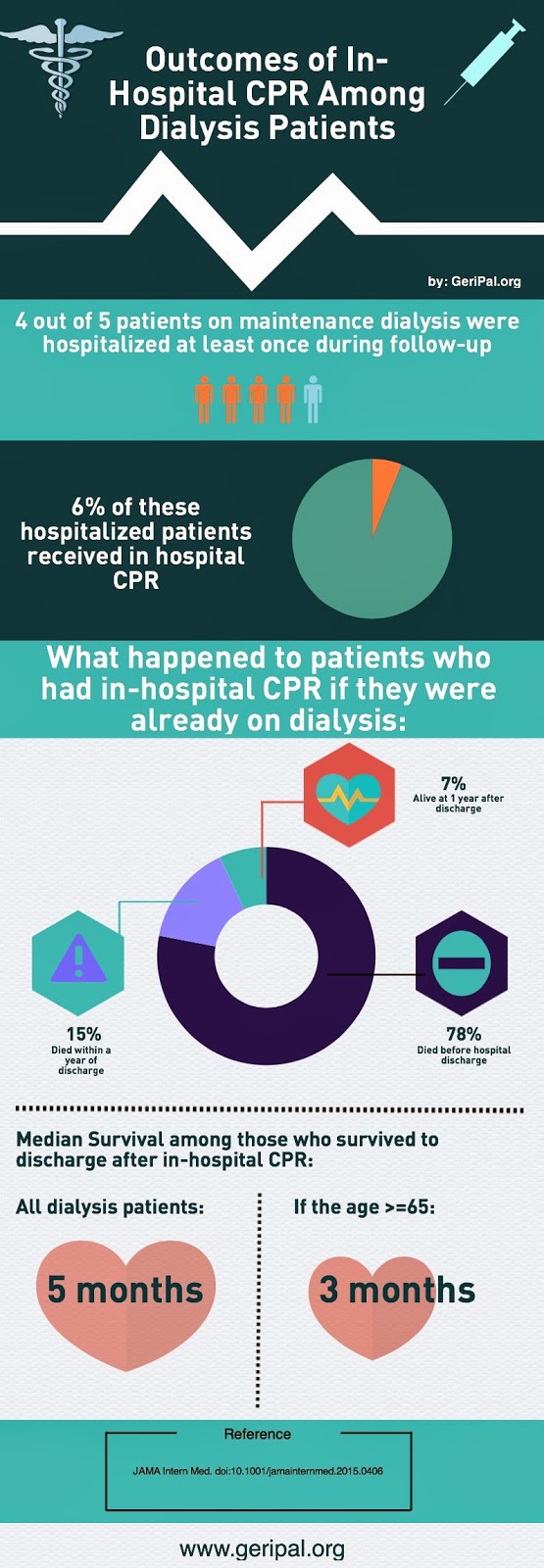
Melissa: Yep. Essentially, what we were interested in looking at was what proportion of … We used United States Renal Data System, which essentially includes all patients who have received, who have end stage renal disease, whether they’ve had a transplant, or been on any form of dialysis and so we looked at this cohort of decedents. These were all patients who had died and we looked back at what proportion of them had received hospice, and then amongst those that had received hospice, how long had they been in hospice. Essentially, we found that only 20% of these patients were receiving hospice services when they died and 42% of them were in hospice for three days or less which, comparing to overall Medicare populations, is about twice the proportion of patients who have these really, really short stays and they’re also about half as likely to be in hospice at all.
Alex: So there are kind of two main headlines, if I could just reiterate the two main findings here. The first one is that, what is it, like one in five, 20 what percent?
Melissa: 20%. One in five.
Alex: Yeah. So about one in five patients who are on dialysis enrolled in hospice before death, so just one in five.
Eric: Which is a significant increase from 2000.
Melissa: Yeah, yeah. We did look at some trends over time and sort of similar to what’s been going on in the general Medicare populations there’s been huge growth for both patients of all different diseases in the use of hospice. What hasn’t changed, both for the overall Medicare population and certainly for our population, is there’s been kind of this no change in the high proportion of patients who are in hospice for a really short time.
Alex: But I think that one in five may be an important number, too, because to me that seems low. I wonder what overall rates of hospice are, A: for overall Medicare population, people who die who are Medicare eligible, receiving Medicare and then, 2: what the proportions are for people with other serious conditions like cancer? How many people with cancer in Medicare receive hospice prior to death?
Melissa: Yep, yep. The 2014 data, 48% of the Medicare population received hospice prior to death.
Alex: So about half. So you’re talking about one in five versus half. These people-
Melissa: One in five versus one half, yeah.
Alex: Yeah, that’s a huge difference, considering that these people are on dialysis. These are seriously ill individuals. That means that there’s some sort of barrier there. There may be many factors in that barrier, but one of them is likely this issue about Medicare not providing a mechanism that’s feasible for funding both hospice and dialysis at the same time.
Melissa: That’s right. I do think it’s important the point you make there. I think that the policy is just one factor. I think there’s a lot of reasons why patients with end stage renal disease are less likely to use hospice than patients with other diagnoses, so I don’t know that if we all of a sudden changed the policy that all of a sudden we’d have comparable numbers or comparable proportion of patients with end stage renal disease.
Eric: So what do you think the other factors are?
Melissa: I think there’s a number of factors. I think patients often, with end stage renal disease, don’t have a sense of how sick they are. In other research that we’ve done we asked, “What do you think the chances are you’ll be alive in a year?” The majority of them said, “Oh, over 90%.” So I think that there’s this perception that, “Oh, well, I’m on dialysis. There’s a machine that takes care of my kidneys. That’s my issue, so I think I’m good to go.” I think in part that is, as clinicians, I think we’re not having conversations about prognosis. I think that … Yeah.
Alex: Are the nephrologists having those conversations?
Melissa: Right. They’re not. They’re not. So in that same study, we found that asking patients, “Has your doctor talked to you about this?” less than 5% of patients had had conversations about their individual prognosis. Their doctor had not shared an estimate of prognosis with them. Nephrologists are pretty open about this as well, that they aren’t talking about it and, interestingly as well, when you ask them, “If a family asked you for an estimate for themselves?” nephrologists don’t feel comfortable sharing.
Alex: I want to go back to the other key finding from your paper, which is that only one in five used hospice, A, but then when they did use hospice, they tended, a substantial group of them used hospice for a very short period of time.
Eric: Nearly half. 41%, 42%.
Alex: 41% for less than, three days or less?
Melissa: That’s right. That’s right.
Alex: That probably also is driven, I think you’re assuming here, by people stopping dialysis very close to death, then starting on the hospice benefit. Is that the kind of driver, or what are the other factors that lead to that?
Melissa: I think that’s right. I think it’s both policy and also models of care. I think patients that are on dialysis, they get wrapped up in a very high treatment intensity when you look at other measures like the intensive care unit. They’re a group that has really high health care utilization and I think that they’re, often they kind of, my sense is, not being a nephrologist, but having spent some time with colleagues that are nephrologists and spending time in dialysis units, it’s like there’s kind of this culture that’s very aggressive and then it’s kind of until there’s something else, a medical crisis, almost like they’re dying from something else. At that point it’s kind of the first time that things change in terms of treatment intensity.
Eric: I think the other things is, especially if … First of all, you did not include those people who started dialysis in the hospital in the ICU for a couple days and stopped, right?
Melissa: Right. These were all patients who had made it into the USRDS and in order to be in that registry, you have to have received dialysis in an outpatient setting.
Eric: Okay. The other question is for these people who’ve been in maintenance dialysis in the outpatient setting, one of the things that we’ve seen here is that the dialysis unit becomes their family, becomes their social network in a way. They don’t view dialysis as sometimes a medical intervention but as, “Oh, it’s a thing that I come to on Monday, Wednesdays and Fridays and I meet my dialysis nurses and I talk to the other dialysis patients”. So I just wonder how much is that playing a role?
Melissa: No, I think we often think of dialysis, initiating dialysis, as the worst thing in the world for somebody’s quality of life, but as you sort of allude to, there’s definitely stories, patients I’ve seen who are socially isolated and they start dialysis and it’s actually sort of a form of socialization, a community, so I think that sometimes, yeah, there’s … I don’t know. Kind of stopping there, but-
Alex: That’s one of the factors. But here’s another suggestion, Melissa. I’m interested in your thoughts on whether this is a factor.
Melissa: Yeah.
Alex: The decision to initiate dialysis, for some patients, may be a marker of underlying values and preferences that dialysis is a life sustaining intervention. If they’ve selected that once, might they be selecting that at multiple stages along the line and so might just by looking at people who are receiving dialysis, examining a group of people who have underlying values and preferences aligned with receiving life sustaining treatment that may … Eric’s looking at me like, “Where are you going with this?”
Eric: No. I like this. It’s like a marker of the goals and values, right?
Alex: Yeah, marker of goals and values that may not align with hospice for some of those folks in some situations, right?
Melissa: Yeah. In the United States, the vast majority of people do start dialysis, so I don’t think that we are selecting for, “Oh, these are the kinds of people who would do absolutely anything to stay alive.”
Alex: And that’s because we don’t have a good alternative at this time of like what is supportive care without dialysis?
Melissa: That’s right. That’s right. I think that is true and there’s really good people working on building models of care. I do think that even with solid supportive care in place, there’s going to be a really large group of people who their goals and values, they want to take a crack at dialysis and they are also frail and likely to die in six months and that it’s not always inconsistent to start dialysis.
Alex: Okay. I have a follow up. Here’s another idea. Maybe because dialysis is pretty much the only option, we don’t have a good supportive care system in place for people who have end stage renal disease or whatever we’re calling it now, chronic kidney disease, that by starting dialysis and offering it as the only option we train people that when you have an organ that is failing, we have a life sustaining procedure for it. And we train people, in a sense, to sort of indoctrinate them into this, there is a problem, we can fix it with our technology sort of mindset so that we are transferring some of those goals and values of our technology driven Western system to those patients. Eh?
Melissa: I think there’s definitely some truth to that. I do think that there can be an on/off switch, like, “Okay, you’ve bought into this, you have bought into it all” when you think about something like code status and dialysis. There’s a qualitative study, a very illustrative quote about a dialysis nurse who was like, “There should be no such thing as DNR, DNI in a dialysis unit. They’ve signed up for wanting to live, so they can’t make …” I can’t remember exactly the quote, but essentially.
Eric: It’s like the post-op setting and the covenant that surgeons feel that patients go into.
Alex: Right. Gretchen Schwarze wrote about this.
Eric: Yeah.
Alex: Yeah. The covenant between surgeons and patients.
Eric: Yeah, you’ve elected the surgery, you’re going to elect really a lot of aggressive interventions post-surgery too, even though that’s not discussed.
Melissa: Right, right. But I don’t think the answer is just, “Well, you …” Because I think we’re kind of doing the same thing if we tell people, “Okay, if you don’t want those things, then you don’t want dialysis. You want conservative care, supportive care”. Because I do think there’s going to be people in that zone where they want to do at least a trial of dialysis, but if things do not go, sort of hoping for the best but not getting on the train to ride on for aggressive care till the last stop when things don’t go well.
Eric: What else did you find in your paper?
Melissa: We also looked at the Medicare costs for patients with different length of stay in hospice and found that with longer length of stay in hospice, Medicare costs were lower and that these really short stays of three days or less were actually more expensive than not having hospice at all.
Eric: Oh, wow.
Melissa: So that was another.
Eric: So having a length of stay in hospice less than three days actually costs Medicare more money than if they didn’t elect hospice at all.
Melissa: That’s right. That’s right.
Eric: So what’s the answer here? What do we do with this?
Melissa: I think that we need to come up with more flexible models of care and this isn’t for patients with end stage renal disease and we’ve spoken about some of that in terms of having a better supportive care track available, but I don’t think that’s the end. I think we also need to have more flexible models of care for patients who are going to do dialysis or at least a trial of dialysis. What does a time limited trial look like? It’s thrown around a lot in the nephrology community in sort of, “Oh, time limited trials”. But what are those and what are the benchmarks that we’re using in terms of circling back to whether continuing dialysis makes sense? And then, for those that are going to continue on with dialysis, how do we think about transitions when things aren’t going as well and breaking down this on/off switch around interventions? I do think that we hope that our … We do hope that it would inform a policy discussion about the potential idea of concurrent care of not making these patients make the terrible choice between continuing dialysis and getting access to what we know is a package of services with hospice that has a lot of benefit for patients and families in terms of improving quality of life.
Eric: Do you think that needs to be done through hospice, or are there other mechanisms like palliative care consult inpatient/outpatient, potentially in this population outpatient integrated in dialysis clinics? Do you think that’s a potential solution?
Melissa: Absolutely. Palliative care is absolutely critical in its ability to meet these patients upstream of these sort of end of life … Palliative care is available to patients with advanced serious illness at all stages of disease and I think that early integration of palliative care is a big piece of this.
Eric: So you actually did a paper about this in JAMA IM, looking at palliative care, whether or not in different diseases people received palliative care in veteran populations and then associated that with things like quality of end of life care. Can you, do you remember that and can you tell us a little bit more?
Melissa: I do. I do remember it, yeah.
Eric: Just making sure.
Eric: Alex one time wrote a paper and then took a boards exam question-
Melissa: And missed his question?
Eric: He got the question wrong and they cited his paper.
Alex: Oops.
Melissa: I don’t have enough papers to be able to have that happen to me, but-
Eric: Sorry, Alex, for outing you.
Melissa: Essentially, in that paper we looked at patients with different serious illnesses and looked at the rates of palliative care consultation and other sort of markers of high and low quality of care. This VA study, the Bereaved Family Survey, is a really rich study because it asks family members about how would you rate the overall care that your loved one received? They ask a lot of other questions, too, but that particular question we saw that patients with organ failure both had much lower rates of palliative care consultation and also lower rates of their family members reporting the care was excellent and when you looked at that association between diagnosis and rated quality of care, once you factored in palliative care consultation, the differences were gone, so making the argument that palliative care consultation can really improve quality of end of life care.
Eric: That’s great. Well, before we go-
Melissa: I was just going to say, on the palliative care front, I feel like a really important message for clinicians is while there is this barrier to accessing hospice, that barrier does not exist for palliative care, so it’s definitely, if our paper does nothing else than to raise awareness about this patient population, I do think that palliative care involvement is critical and that there is not a policy barrier to that. That said, I do think that there is added benefit of having hospice services as things start to get worse, but not necessarily having to wait until they stop dialysis. Service that’s available to people literally in the last days of life, so I do think the added benefit being that access 24 hours a day to a nurse, the bereavement services, there are things that hospice is added benefit beyond just palliative care.
Eric: I really want to thank you for joining us on this podcast.
Alex: Thank you, Melissa. Appreciate you joining us. This was fun.
Eric: It’s great chatting with you. Maybe to end us, Alex, can you give us a little bit more of that song?
Alex: Little bit more of “Running Down a Dream” by Tom Petty.
Melissa: Yeah.
Alex: [Singing]
Eric: Nice.
Alex: So, anything else you want to say, Melissa?
Melissa: I do feel like for this population, essentially we’re asking them to make a decision to stop dialysis in order to get hospice. We think about cancer patients as a population, we’re often talking about hospice and essentially, as people die within days to a week after stopping dialysis, it would be like saying that patients with cancer can’t get hospice until they stop taking any oral fluid. I think that it’s kind of stark in terms of, “Well, we’re not going to give these services until it reaches a certain sort of end point” when, of course, all hospice days could be, we know overall the median length of stay in hospice is relatively short. Everyone could probably benefit from a bit longer stay. I do think that it really, for this particular population, we’re really limiting it to the final days of life, which don’t think we … I don’t know. It’s just, again, it’s not treatment, but-
Eric: I think the hard part is it’s really not about, nobody’s saying they can’t do this intervention. It’s like the chemotherapy question where it’s about financing. Who needs to pay for this intervention, which is really the limiting thing. It makes it, in all practical ways, it’s as people can’t continue dialysis if it’s their terminal illness or related to their terminal illness.
Alex: Right. The financing serves as the barrier.
Melissa: Yeah. Yeah.
Eric: The financing serves as the barrier, but nobody says … Because we do a lot of disease modifying therapies in hospice, like everything that we do for CHF in hospice like we’re continuing their diuretics and it’s this old traditional way of thinking, breaking down the body into organs instead of a holistic approach to the person that doesn’t make a lot of sense.
Melissa: Right.
Eric: That’s probably the thing that we should challenge. It’s more about the needs of the person rather than a need of an organ.
Melissa: Totally. Totally agree. Thank you guys. This was really fun.
Alex: Thank you, Melissa. Appreciate you joining us.
Melissa: All right.
Eric: And thank you to all the Geripal listeners out there. We look forward to talking with you next week.