by: Alex Smith @alexsmithMD
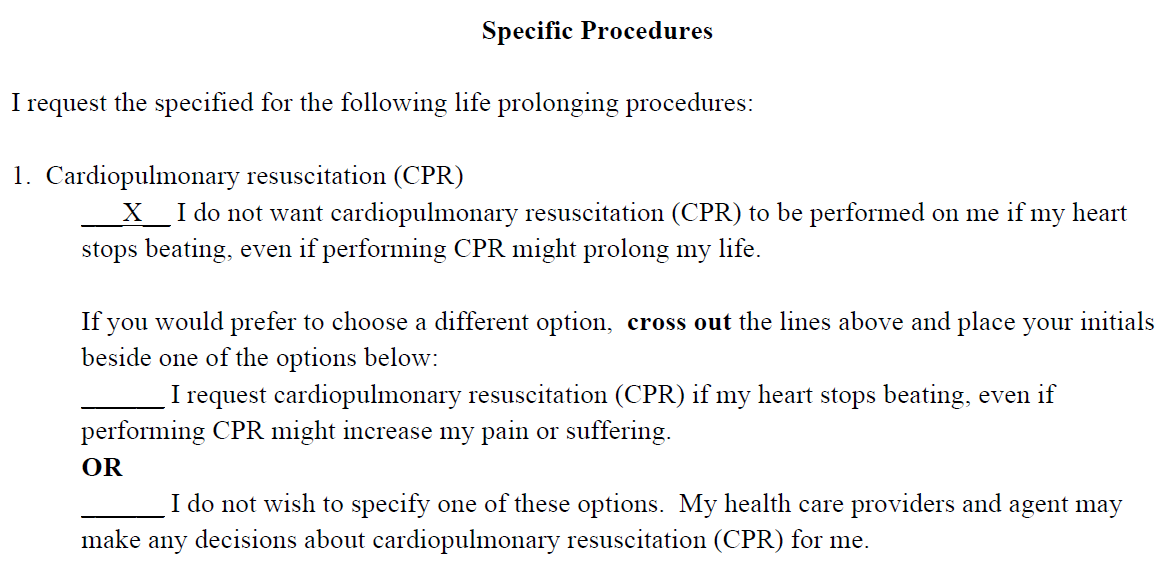
What if the above form was the default for patients with serious illness? Most current advance directive forms and the POLST have no default – although one could argue that our default without a form is full code. But what if we could set a default on these forms, so that when a patient received a diagnosis of a serious life limiting-illness, the default option was Do Not Resuscitation (DNR)?
Scott Halpern and colleagues tried this approach in a study published in Health Affairs of 132 seriouly ill outpatients with incurable diseases. Patients were randomly assigned to complete one of three advance directives:
- Comfort default: default of DNR.
- Life-Extension default: default “full code.”
- Standard advance directive: patients chose preferences for rescusitation.
Patients in the two “default” pathways could change their advance directive by crossing out the default, initialing the cross out, and selecting another option. You can see examples of all three advance directive forms in the appendix.
What did they find?
- Nearly 80% of patients in the comfort-care default accepted the default.
- 61% in the standard advance directive chose comfort care
- 43% in the life-extension default crossed out the default and changed to comfort care
- After explaining the manipulation of the study forms into 3 possible advance directives, only 2.1 of patients changed their selection. People were pretty content with what they selected the first time around.
- Satisfaction with the advance directive form was high for all 3 versions of the form.
What’s it all mean? Defaults matter. Defaults are part of the behavioral economics revolution, a subject we’ve discussed previously on GeriPal. This study suggests that peoples preferences for resuscitation are not deeply held, they are highly influenced by the (somewhat) arbitrary choice of the default options. This may be true because people have very little previous experience to ground their preferences, and often have no idea what sort of care they would prefer in a future state near death.
Should we change the default choice for patients with seriuos life-limiting illness to DNR? Why not? Seriously. As long as you give the patients a clear path out of the default, why not?
To be sure, the forms matter far less than the discssion. But let’s not kid ourselves here, folks. Even if we try our best to educate all clinicians about how to have high quality discussions, the forms matter. Forms will inevitably be used to guide the discussions and influence patient choices.
So I’m waiting to hear of the first health system to try it. Once we have one or two, others will be brave enough to follow. Why aren’t we changing? Because, as this study shows, it’s hard to go against the default!
NOTE: This is the second in a series of posts this week for “Code Discussion Week.” Come back everyday this week for a new post focused on CPR AND DNR Discussions.
Here is a running list:
- It’s all in the Framing: How to Influence Surrogates’ Code Status Decisions
- Changing the Default Code Stus to DNR for Seriusly Ill Patients
- The Clinician as the Choice Architect – Nudging an Informed Choice About CPR
- What Is A “Natural” Death, Anyway?
- Discussing CPR: What Makes It So Different?
- CPR Discussions and Harm Reduction
- When Not to Follow an Advance Directive



