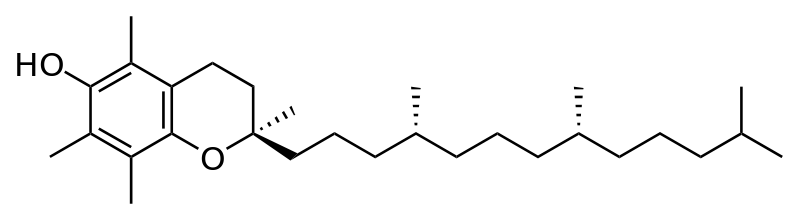
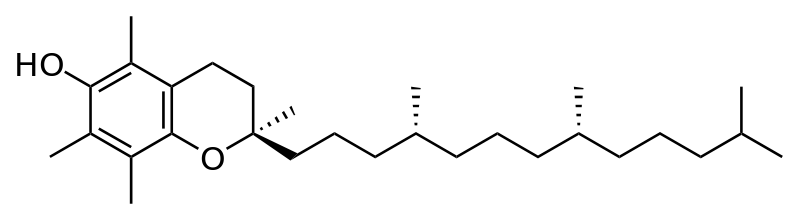
Alpha-tocopherol (vitamin E) and dementia have had a long and confusing history. For the prevention of dementia, Vitamin E has generally been shown to be ineffective over follow-up periods that ranged from 7 to 10 years. Even more concerning, higher doses (more than 400mg a day) have actually been shown to increase mortality (in one meta-analysis the all-cause mortality risk difference in high-dosage vitamin E trials was 39 per 10,000 persons).
For the treatment of dementia, Vitamin E’s story is even a little murkier. There was an Alzheimer’s Disease Cooperative Study (ADCS) randomized control trial of Vitamin E (alpha-tocopherol) , selegiline (a monoamine oxidase inhibitor), both, or placebo in adults with moderately severe Alzhiemers disease. There was no significant differences in the primary outcomes, however the authors argued that they needed to make statistical adjustments since the placebo group had higher MMSE score at baseline. After adjustment, the authors found a delayed progression to outcome in the vitamin E group. This trial left a lot of uncertainty on what to do with Vitamin E, especially given the mortality concern. This confusion is somewhat cleared up by the TEAM-AD VA Cooperative Randomized Trial published this week in JAMA.
TEAM-AD VA Cooperative Randomized Trial
This was a randomized clinical trial in older veterans with Alzheimers disease with MMSE scores ranging from 12 to 26, all of who were receiving acetylcholinesterase inhibitors. The participants were randomized to 4 treatment groups:
- Vitamin E (alpha tocopherol) at 2000 IU/day
- Memantine 20 mg/day
- Vitamin E and memantine
- Placebo
The primary trial outcome was about function using a score on the Alzheimer’s Disease Cooperative Study/Activities of Daily Living (ADCS-ADL) Inventory. This s a 78 point score, so a 1 point improvement may be statistically significant but also may have no clinical significance. The authors suggest that a 2 point change may be meaningful as “it potentially represents, for example, a loss of dressing or bathing”. Secondary outcomes included two cognitive measures: the MMSE and the Alzheimer’s Disease Assessment Scale–Cognitive subscale (ADAS-cog), one measure of psychological and behavioral problems (the Neuropsychiatric Inventory), and a measure of time caregivers spend assisting patients with Alzheimers (Caregiver Activity Survey) (CAS), and the Dependence Scale,which assesses 6 levels of functional dependence.
Results
613 veterans (mostly male) were randomized to the four groups and followed for a mean of 2.27 years. 256 participants didn’t complete the trial, mainly because 128 died during the follow up period, however withdrawal rates were similar among all treatment groups.
Primary Functional Outcome (ADCS-ADL Inventory)
Compared with individuals assigned to placebo, those assigned to vitamin E alone experienced 3.15 units less functional decline on the ADCS-ADL Inventory (95% CI, 0.92-5.39; adjusted P = .03).
There was no statistically significant difference in ADCS-ADL score for memantine or the combination group versus placebo (I must say the graphs looked pretty much the same to me for most of the treatments).
Secondary Outcomes
None of the groups differed on the ADAS-cog or the MMSE. Vitamin E did have a statistically significant improvement over memantine on the time caregivers needed to spend assisting patients with ADLs (2.17 hours less in the Vitamin E group).
Safety
There was no significant increase in mortality with vitamin E compared to placebo. “Infections or infestations” occurred more frequently in the memantine and the combination group compared with placebo (although I can’t say I’m sure though what the authrs mean by an infestation).
What to do with this information
1) Vitamin E may have some very modest benefit on daily function, but it is unlikely to improve cognition based on this study. Like cholinesterase-inhibitors for dementia, vitamin E gives at best a statistically significant but modest clinical benefit in individuals with mild to moderate disease. However, this shouldn’t be generalized to others as evidence suggests that Vitamin E does not prevent dementia in cognitively normal adults or those with mild cognitive impairment (MCI).
2) Don’t prescribe memantine for mild to moderate dementia. This is just one of several studies showing memantine doesn’t really do anything for those with mild to moderate dementia (despite previous attempts by authors to paint some of these articles in a very positive light despite negative results). Also, in this study the combination of vitamin E and memantine was less effective than vitamin E alone. For a good review you can read this meta-analysis (http://www.ncbi.nlm.nih.gov/pubmed/21482915).
3. The need for Advance Care Planning. Why? 1 out of 5 particants die within a median follow-up time of 2 years. I’ll leave it at that.
by: Eric Widera (@ewidera)
Note: for a great review on this article check out Pam Belluck’s article published in the NY Times the New Old Age Blog



