by: Eric Widera (@ewidera)
——
Note: for the most up-to-date information on prognosis in COVID, please go to the GeriPal COVID Prognosis page (now including some outcomes on CPR in COVID).
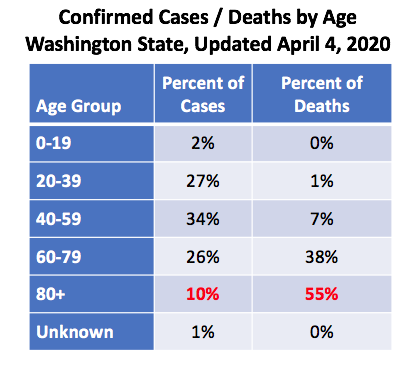
COVID-19 data out of Washington for older adults is sobering: only 1 out of 10 cases are in individuals who are 80 years and older, yet this age group accounts for 55% of all deaths. If you group all adults over 60, they make up a third of the confirmed cases and a staggering 93% of all deaths.
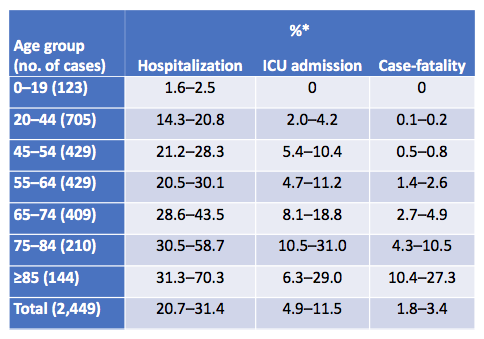
Data from around the US also shows that age is a strong risk factor for hospitalization, ICU admission, and mortality. The following is data coming from CDC looking at US cases from February 12 to March 16th.
Around the world, the numbers look about that same too, with a case fatality rate around 15-20% for those 80 years and older (data from Lancet and JAMA).
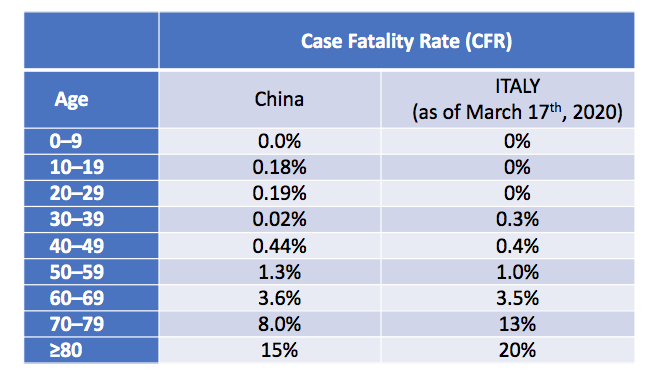
Case fatality rates are defined as the number of deaths in persons who tested positive for SARS-CoV2 divided by number of SARS-CoV2 cases. The case fatality rate is a hard number to pin down due to a lot of factors, such as only the sickest cases early on get tested which likely worsen case fatality rates, but also data on age and outcomes tend to be missing, which can underestimate these outcomes. Also, one needs time to follow-up on outcomes, and with extended ICU stays that we see with COVID, we really don’t know real death rates until weeks (maybe a month) after symptoms arise.
Importantly though, just because someone is older, doesn’t mean that they will die from this virus. The majority don’t. Even if you look at nursing home populations, the majority are alive (at least at the time of reporting). For example, lets look atdata coming out of one King Country nursing facility published recently in the NEJM. The median age of the confirmed COVID case was 83. Over half were hospitalized and 34% died. However, 66% were still alive at the time of reporting.
What about those who were sent to the ICU?
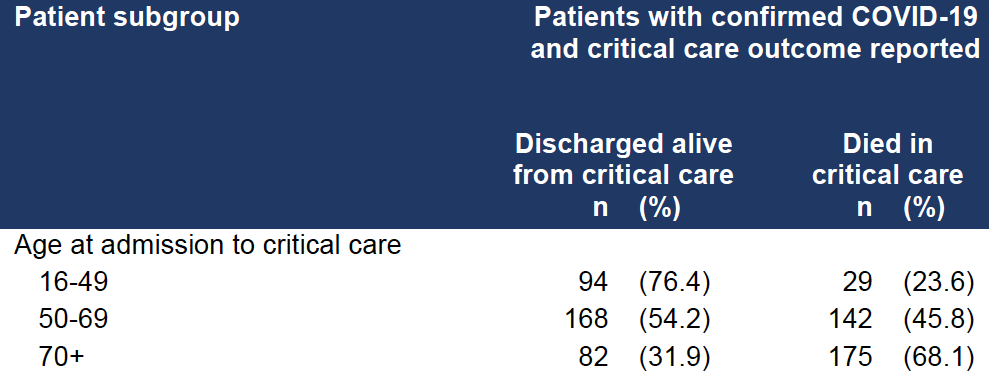
These numbers are even harder to define because of the long clinical course in the ICU for many patients means that we don’t have any clear data. For example, a lot was made out of the ICNARC data looking at critically ill patients in the UK. Lots of folks focused on the fact that 346 patients had died and 344 patients were discharged alive. On quick glance, that’s a 50% mortality rate. However, most patients were still in the ICU at the time of reporting (1559 out of the total 2249 patients). So the data is really to early to give any indication of what the real ICU mortality rate is. But if you just look at those 70 years of age and older who had data reported on outcome (i.e they were not still in the ICU), 32% were discharged alive (again, take these #’s with a huge grain of salt, as most were still in the ICU at the time of reporting).
Outside of this study, I only know of two smaller studies that seem to confirm a high mortality rate (send me more if you got them). If you look at one report out of China looking at 52 critically ill adult patients with SARS-CoV-2 pneumonia who were admitted to the intensive care unit (ICU). They found 62% died at 28 days, with a median duration from admission to ICU death of 7 days for non-survivors. The numbers were worse for those requiring mechanical ventilation (81% requiring mechanical ventilation had died by 28 days). But these were early data, so be cautious about extrapolating this data.
We also see similar high mortality rates in the ICU out of early data from Evergreen hospital in Washington state looking at 21 critically ill patients with COVID-19 with a median age of 70. As of March 17, mortality was 67% and 9.5 were discharged from the ICU. However, 24% of patients remained critically ill, so the overall ICU mortality rate is somewhere between 67% and 91% depending on what happens to these individuals. We do know that the majority of these 21 individuals were linked to exposures at a skilled nursing facility, so we don’t really know what the overall ICU rates look like yet for the general population, but it certainly does not look good for older nursing home patients.
So what is the prognosis in COVID infections?
So to sum up what I know about prognosis with COVID (I’m hoping other’s may know more – please add to the comments section or reply to me on twitter):
- For those in the community, we know if you get it, there’s probably a 50% chance you don’t know you have it as you may be asymptomatic. Even in nursing homes, it looks like at least initially 50% of patients are asymptomatic (listen to our podcast tomorrow for more on this). And if someone does get tested and it comes back positive, the majority of individuals, including older adults will be not die from the virus.
- We know things look much worse if you get admitted to an ICU and require mechanical ventilation, but we don’t have a lot of data yet to see what’s really happening in this setting (if you got #’s, send them my way!) My best guess is that for older adults who require mechanical ventilation, the overall mortality rate is probably well over 50% but less than 90% (I know, big range, but that’s all I got for now).
————————————————
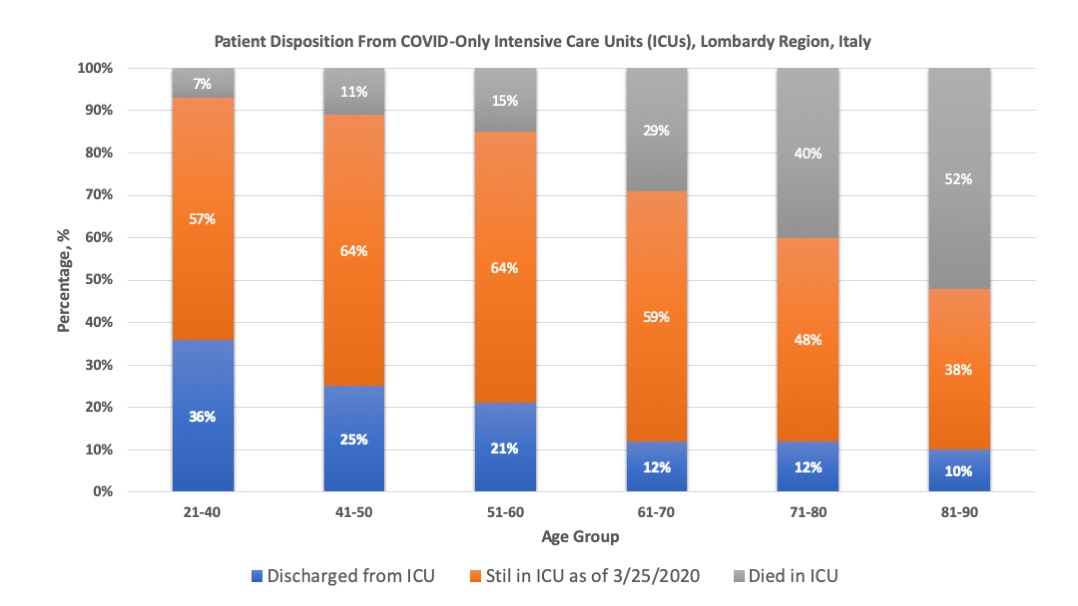
UPDATE 4/6/20: New data on disposition from COVID-only Intensive Care Units (ICUs) in Lombardy Region, Italy shows similar numbers although many still remain in the ICU(orange bars) making this still very preliminary.
———————————————-
NOTE: If you want more GeriPal COVID content, including podcasts with front line providers in Seattle and New York, check out our new COVID page.



