While palliative care most traditionally grew up with a strong association with cancer care and end-of-life care, more and more evidence is coming out about how to integrate palliative care into a variety of serious illnesses from heart failure to chronic lung conditions. Another emerging field is the integration of neurology and palliative care, something that has been coined as “neuropalliative care.”
We had Benzi on a previous GeriPal podcast to talk about palliative care in Parkinson’s disease. On this week’s podcast we go much deeper into the field of neuropalliative care by inviting leaders of the new field and in the International Neuropalliative Care Society (INPCS), Benzi Kluger, Edward Richfield, and Christine Ritchie. INPCS connects clinicians, researchers, interdisciplinary team members, people living with neurological illness, family members, and advocates at the intersection of neurology and palliative care.
In addition to talking about why INPCS was developed, we talk with these leaders about:
- What are the unique palliative care needs of patients with neurological conditions and their family members?
- Do we really need a society focused on a subspecialty in palliative care and do we need it for every subspecialty in palliative care?
- How can palliative care be integrated into neurology practice?
- What are the gaps in the field of palliative care when addressing the needs of patients with neurological diseases?
- What are some key lessons learned doing neuropalliative care on how to care for patients with neurological diseases?
One other big shout out too for INPCS is for their inaugural Annual Meeting on November 4-6, 2021. The online conference will offer attendees the opportunity to learn from experts, hear updates in practice patterns, review the state of the science in neuropalliative care, and network with others interested in this growing field. Best part, it’s free! So sign up.
Eric: Welcome to the GeriPal Podcast. This is Eric Widera.
Alex: This is Alex Smith.
Eric: And Alex, who do we have with us today?
Alex: Today, we’re delighted to welcome back Benzi Kluger, who is Professor of Neurology and Medicine at the University of Rochester, and also directs the Neuropalliative Care service there; and is the President of the International Neuropalliative Care Society. Welcome back to the GeriPal Podcast, Benzi.
Benzi: Thanks for having me back.
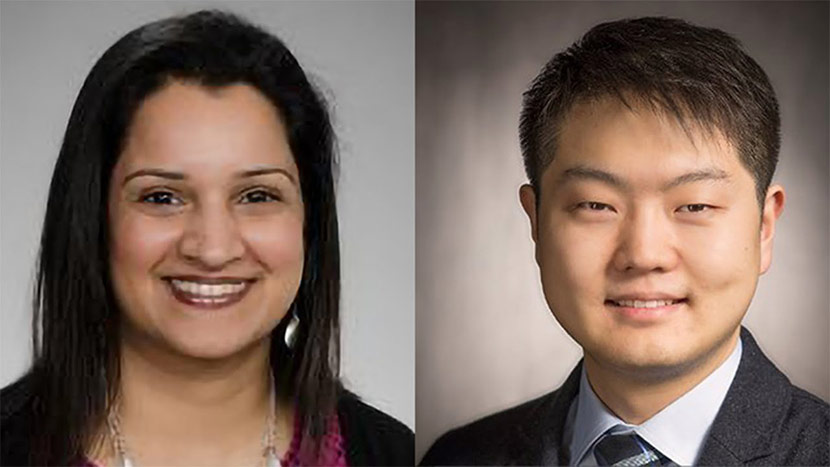
Alex: And we are delighted to welcome Christine Ritchie, who we’ve been trying to find a date for forever and we finally found one that she can join, so this is terrific. We’re so thrilled to have you on. She’s Professor of Medicine in MGH and Harvard Medical School, Massachusetts General Hospital that is MGH, and Director of the Center on Aging and Serious Illness; and a board member of the International Neuropalliative Care Society. Welcome to the GeriPal Podcast, Christine.
Christine: Thanks, Alex. It’s really great to be here.
Alex: We have from the UK joining us is Ed Richfield, who is a consultant geriatrician in Bristol, and chair of the Clinical Committee for the International Neuropalliative Care Society. Welcome and thank you so much for joining us today, Ed.
Ed: Thank you. Thanks very much for having me.
Eric: Sounds like, Alex, we have a theme, international neuropalliative care. So we’re going to be talking about that theme throughout this entire podcast. But before we do, we always go to a song request. I forget, who are we turning to, Alex, for the song request?
Alex: I think Benzi or Christine.
Eric: Benzi?
Benzi: I’ll take it. I think Christine and I have a similar idea for a song. We both love the Beatles. With the theme of neuropalliative care and this international society, we felt like Come Together would be a great song for launching the podcast today.
Alex: Great choice. Here’s just a snippet at the start. (singing)
Eric: That was excellent.
Eric: First of all, thanks everybody for coming. We had Benzi on in 2020 to talk about… Right after he published as, I think, lead author, JAMA Internal Medicine paper on Parkinson’s and Palliative Care: A Randomized Controlled Trial; encourage all of our listeners to check that out.
Eric: We had a chance to talk to Benzi about, first of all, what got him interested in neuropalliative care. That’s going to be the subject today. So, I’m hoping to turn to Christine and Ed to really start off the discussion about why they got interested in this.
Eric: Then we could talk about is this a specialty unto itself? Do we need a whole other society on it? Just learn a little bit more. Maybe at the end, we can hear some practical tips that we can bring in to our own practices.
Eric: But Christine, you’ve been a figure in both geriatrics and palliative care nationally in the US, internationally. How did you get interested in neuropalliative care?
Christine: Thanks for asking, Eric. As a geriatrician and a palliative care physician, this is the space we often occupy, which is the space of caring for people living with dementia across the care continuum.
Christine: Actually starting with my time at the University of California, San Francisco, I had the opportunity to spend more and more time with my colleagues in neurology and psychiatry, geriatrics and palliative care. All of us bringing important pieces to the puzzle, and yet still staying maybe more in our own lanes than was helpful. Seeing the opportunity for better care in this space was part of what drove me to it.
Christine: Also, because palliative care has historically been more in the oncology world. Thinking about how we might bring it more into the world of neurology and dementia care was attractive to me.
Christine: Then last, but not least, my father had Lewy body dementia, and I had the privilege of caring for him in the last years of his life in my home. That certainly spurred on a deep desire to do work in this area.
Eric: Thank you, Christine. How about you, Ed?
Ed: Yeah, so thanks for having me on. I guess just my day-to-day work as a geriatrician we see a ward full of older people, actually younger people as well now with frailty and multimorbidity, and within that we see lots of folks who’ve got neurological conditions often combined with frailty syndromes and multimorbidity. We tend to see people after they’re admitted to the hospital so often at a point of crisis in their life.
Ed: And often… I think that’s really when the feel the absence of prior palliative care so for instance where they haven’t had any particular planning, people haven’t discussed goals of treatment and so forth. Lots of our job would be this in general geriatrics talking to folks and families and trying to work out in your best interest decisions because folks have maybe lost the ability to take part in conversations, set their own goals of care. I think as geriatricians our work in the ward everyday you very much feel that role for palliative care in its wider sense and the absence of it. You really sort of feel for families and patients and you sort of live it with them and the problems around that. That was sort of my clinical background, then the opportunity came up to do a PhD with palliative care and Parkinson’s disease. I was already subspecializing in movement disorders so it seemed like a natural fit for me. You kind of think, well as a geriatrician if you’re not going to take the opportunity to take three years to look at that then probably time to get another day job. Too good of an opportunity to just mess with me so that was my way into this as a specialty.
Eric: Can I ask, International Neuropalliative Care Society, institute?
Benzi: Society
Eric: Society, when was that dreamed up? When did it start?
Benzi: It was born… I guess the idea goes back maybe five years. There was a group of us in the American Academy of Neurology who had an international neuropalliative care what we were calling a summit and it was four hours on an afternoon, in an outside hotel because we didn’t want to pay to be official, and it built up over that four years. The last time we held it there were over 100 people who joined from all over the world. It was building momentum. I think at that time within the American Academy of Neurology there was a pain and palliative care section which is now a palliative care section we split off. It seemed like we weren’t really able to do what we wanted to do within that section. We wanted greater networking.
Benzi: I think one of the things which goes into why there’s two geriatricians and a neurologist here is that I think we all recognize that we really needed it to be interdisciplinary. I think all of us clinically, research, education, were collaborating with geriatricians, we were collaborating with palliative care, we were collaborating with chaplains, with social workers and there wasn’t any place where we all hung out. We were all interested in what everyone else was doing.
Benzi: The other part of it, the international piece, being interesting also to get Ed takes on it, was… Think it was actually 2012 we had our first international Parkinson’s palliative care working group. We had some people from the UK and Australia. It was just eye-opening to me how different palliative care looked under different systems. There was a huge opportunity for me to learn because prior to that I was working with the US blinders that hospice needs to be based on prognosis. The guy from Australia was like that doesn’t make any sense. It’s based on need here. I was like oh, that makes a lot sense to me. We’ve found that in other work. I think what’s one of the beautiful things here is that by comparing how things are working in different contexts it can actually even push policy with evidence. In the study that you mentioned, caregivers in Canada were doing statistically significantly better at baseline before we started our intervention. That has to do with the social support structure in Canada which I think is an important lesson for us that we can also be advocates and champions for better models of care and not just better direct clinical care.
Eric: When we think about neuropalliative care, how are we defining that?
Benzi: Defining it in terms of, I guess two things, one is recognizing that people with neurological illness have palliative care needs but the reason for calling it neuropalliative is that they’re unique needs. We can have a debate or argue about that. I think if you go across the board and look at pain in patients with neurological illness like Parkinson’s, there are unique causes of pain in somebody with Parkinson’s so symptom management is different, symptom assessment is different. The way it affects somebody’s identity with Parkinson’s or dementia is very different than how it affects somebody’s identity with cancer. The struggles that caregivers have is different.
Eric: I care for people with neurological problems, heart problems, renal problems, pretty much every organ system. Does there need to be an international society of cardiac palliative care, international society of renal palliative care, and do I have to belong to all of these societies in order to… Because there are unique needs for everyone of these. How much of this is medicine loves, especially academic medicine, loves super sub-sub-specialization? How should I think about that when it comes to neuropalliative care?
Benzi: For me, again I’d love to hear what Christine and Ed have to say, as a neurologist, part of the reason I’m actually pushing for it is I think there’s a need for ownership. If no one is really owning neuropalliative care and ends up being owned by nobody or it’s kind of deferred to palliative medicine. I feel like if we’re thinking about palliative care as something that’s going to be done proactively, if we’re thinking about primary palliative care as something that’s going to start at the time of diagnosis, something that’s going to prepare caregivers that there needs to be some ownership there to move forward as a field, research-wise, but even clinically. It feels very important that neurologists and others, geriatricians, that other people take some ownership for it. This may be true for nephrology. It’s probably actually needs to be done more for cancer. If people are not taking ownership for it they’re not integrating it, they’re not embedding it in their clinics. As a palliative care doctor, that is one perspective on it. As somebody closely associated with the disease, if I’m not owning and associating with palliative care and it’s not my job, it’s not going to move forward very fast at all.
Ed: I think one of the big differences cognitively is that the opportunity to… we all buy into the fact that palliative care can and should start, as appropriate, from the time of diagnosis. I think it’s even more important in conditions where there’s a high cognitive burden because of the loss of autonomy. If, as you say, neurologist or geriatricians or whoever the chronic care physician is, if you like, is not involved in that then those opportunities are lost. Almost by definition then you end up with a more prognostic model of care if folks aren’t identifying needs early on then you’ve lost autonomy for so many people. I think that’s one of the big differences.
Ed: I guess the other thing for me, from my experience as a geriatrician would be there is a generalist subsequent base of my job is as a geriatrician. We have good training and theres other conditions. There’s lots of people feel comfortable managing heart failure and COPD and maybe to a lesser extent renal disease but actually a lot of generalists feel uncomfortable managing neurological conditions. I think the same is true for palliative specialists if they haven’t had specific neurology training. So, people tend to shy away from them. That’s all the more easy now with the call for palliative care for non-malignant disease. If I was working in a hospice, I would naturally move towards COPD and heart failure partly because that’s very vague and partly because that’s conditions I feel comfortable with. The real danger, I think, then that folks with neurological disease would be missed out.
Eric: Anything Christine? When you think about this too, from a dementia perspective, there’s been a lot of talk in palliative care about the palliative care needs of individuals living with Alzheimer’s disease and other dementias and the need for increasing specialty palliative care for those groups. To be honest, we don’t do a super great job of training palliative care specialists on how to take care of people with dementia. I’m wondering from your perspective, how do you think about that?
Christine: I couldn’t agree with you more, Eric. I think part of what’s actually drawn me to this space is seeing that this is a real opportunity for us in palliative care to go deeper, to go richer and to really increase our competence. Part of what I think is attractive about this international neuropalliative care society is that it brings together people who might not otherwise rub shoulders to think about what that looks like. What would providing high quality, highly competent palliative care for people living with dementia look like? It has to come from an array of perspectives from neurology, from geriatric psychiatry, from nursing, from geriatrics, from palliative care, and it’s hard to get all those folks at the same picnic table. Part of it is the opportunity to do that. I do feel like its tremendous opportunity for us in palliative care to go deeper with our training around dementia care.
Christine: I’ll say that in my work here at Mass General where I do a lot of dementia care that discomfort with dementia care, certainly not just for those with palliative care training, there’s generally a discomfort around dementia care. Our opportunity to both normalize the relevance of palliative care and dementia care from the beginning to the end-of-life with our primary care colleagues and with our other subspecialty colleagues is something that is incredibly compelling.
Alex: I wonder if you could talk about what the fields have to learn from each other. I’ll give you an example from outside the field of neuropalliative care. Bioethics, for example, has to learn from palliative care the importance of relationship and building relationship and paying attention to the emotions of the patient and the family members rather than decision dictated from some conference room from on high based on lofty principles. Are there elements that neurology has to learn from palliative care or that palliative care has to learn from neurology in this case? Anyone can talk. I’m just going to throw it out there.
Benzi: I can start. When I got started, Jean Kutner, at the University of Colorado where I was, was really instrumental for me getting things off the ground. At that time, and it’s still the case I think in most cases, palliative care was really not taught or taught well in neurology. I think a lot of program directors checked off the box because we did brain death exams and that’s kind of palliative so we’re doing palliative training for our trainees. I knew almost nothing about it, so it was very helpful for me to learn how palliative care doctors approach symptom management, how palliative care doctors approach advanced care planning. Part of the reason actually I approached Jean in the first place is that I felt very stuck as a neurologist. I would see somebody with Alzheimer’s disease and at a certain point I could watch locomotion go down, I could take away the driver’s license, I could start Aricept, but I really wasn’t doing anything that I felt satisfied with. Talking to Jean and asking her and looking at things through her perspective, gave me a whole new set of tools. I felt helpful again. Without palliative care, I might have burnt out just because… Without palliative care it seems like neurodegenerative diseases are just horribly depressing.
Christine: Maybe just to add to that, in some of the work that I’ve had the good fortune of doing with Krista Harrison at UCSF, we found that a lot of what neurologist do feel uncomfortable with relates to what you just talked about Benzi, which is the communication space and the anticipatory guidance and this sort of weaving together of the complexity and the use of providers with respect to dementia and multimorbidity that those things are diagnosis as sort of bread and butter but theres other pieces of the caring, caring for the caregiver. Those pieces are much less part of the traditional armamentarium so I think there’s a real opportunity there.
Christine: I also think to answer your question, Alex, in the opposite direction what can palliative care learn? I think getting just a little bit more sophisticated in our understanding of dementia, understanding dementia subtypes so that we can actually provide better quality anticipatory guidance, understanding what medications really are highly problematic to provide for our people with cognitive impairment, especially with dementia, or Parkinson’s disease for that matter. Being aware of some of the treatment strategies that are relevant both for supporting caregivers of people living with dementia but also people who have dementia with respect to behavioral symptoms which a lot of folks in palliative care haven’t had a lot of training in. Things like inner drooling, movement disorders, again things that just are not the typical bread and butter symptom management issues for many in palliative care.
Alex: Ed, anything you’d add?
Ed: I agree with all of those. I think that’s one of the nice things about it is the way we all learn from each other. So we have here a Parkinson’s disease palliative care multidisciplinary team meeting which we meet once a month but we quite frequently get phone calls about patients in the meantime and they go three ways. I do think this month I phoned one of my neurology colleagues asking about something that seemed quite odd to me. I wanted his advice. I’ve gotten phone calls from palliative care consultants asking me specifics about drug managements. It works all three ways so it’s actually really good. I think probably one of the biggest lessons that I’ve learned it goes a lot of… Most of our practice now is in hospital so we do have clinics. In hospital a lot of time pressure and through the pandemic and things and actually learning the importance of structures because actually you can have good communication skills and you can care lots and really want to try and do a good job but if you do it in a structure that isn’t enabling it is very difficult.
Ed: I think we have this idea that, maybe it’s in the UK, there’s sort of stereotypes about different specialties. They like doing this or they didn’t feel comfortable doing it. You try seeing about advanced care planning in 15 minutes you can’t do it if your appointments are 15 minutes long. You really can’t do it. It’s about having the structures around you that enable you to do it well. I think that’s probably the biggest thing I’ve learned.
Alex: I have a follow-up question. Ed, when you said all three areas are important I think you’re talking about geriatrics, palliative care, and neurology.
Ed: That’s right.
Alex: Yet, the society is called the International Neuropalliative Care Society. Geriatrics got dropped, so I wonder if they were thinking maybe we should be the International Neurogeripal Society. My followup question to that is, did you decide not to do that because you knew that GeriPal was trademarked and you’d have to pay us thousands of dollars in royalties.
Christine: I love the idea Alex by the way. I do think GeriPal is a really important piece to this conversation. Again, getting back to some of the work Krista and I have done together, geriatrics… What we’re seeing is sort of deficits in a lot of the care provided. It’s sort of an interesting combination of geriatrics and palliative care, so I don’t know we might have to pay thousands of dollars to add that to the title.
Benzi: I would say that we’re having parallel conversations. I think geriatrics is actually a big piece of the puzzle. In the pediatric neuropalliative care space, there’s kind of like a parallel but smaller and cuter universe. It’s a similar thing with kids with complex neurological illnesses and developmental delay and epilepsy and things like that. Again, it’s this kind of no man land where there’s definitely a need and I think people recognize it for interdisciplinary care, interdisciplinary research, interdisciplinary conversations that aren’t happening. Part of the hope is that International Neuropalliative Care Society can kind of serve as a post in a home for geriatrics, neuro-oncology is another space where we are seeing similar things, pediatrics is another. I think we talked maybe even before the podcast started about how we came up with this society so that this could be the main course. Geriatrics, pediatrics, all these other things I think will be task force and working groups and hopefully be part of the bread and butter of this society as it develops.
Alex: I have a question for you. Go ahead Christine.
Christine: Just to add, because we haven’t given much voice to it, is the very important role of geriatric psychiatry. It’s a small field, and yet they offer so many incredibly complimentary perspectives to this space. I think we would be remiss if we don’t at least also talk about the guides that they offer especially around complex behavioral symptoms.
Eric: Who should join the International Neuropalliative Care Society?
Ed: Well, I think that’s really one of the strengths isn’t it that’s emerged in the last year. I think a lot of the societies say it that everyone’s welcome but I think in the INPCS genuinely everyone is welcome and that’s really been set forth from the foundation of this society. Genuinely everyone’s views are really respected and held tightly and a genuine place to learn from each other. I think because it is such a relatively new field and because there genuinely are areas of which each discipline may be outside of medical sense, the multidisciplinary team, are genuinely bringing things which other people go oh yeah, that’s really interesting. People will be bringing things that even like professors in neurology or professors in geriatrics will be saying you’ve added to my knowledge. That’s a really great thing actually. Certainly, we’ve been opening it up to trainees, specialist nurses. There’s so many folks I think that should genuinely feel welcomed to come and join.
Benzi: I think GeriPal listeners would be great members. Ed’s the head of our clinical task force. A lot of our task force I think is speaking to the hunger for a society in this space. There’s definitely a hunger for clinical guidelines and for clinical colleagues to talk things over for people who are trying to get clinics off the ground in the space. Same thing for education, talking to Christine’s points about needing tools and other things for palliative care fellowships, other things for neurology residencies. Research, there’s certainly a lot of opportunity there.
Benzi: One of the other things that’s unique which we haven’t talked about but was important to me as we got this society off the ground was to have a place where patients and families living with neurological illness would be treated as the experts they are and to really have a voice and be integrated into our society. On our board, theres patients, there are care partners. I think for patients and families who want to change the way care is provided and change standards of care that this can be a very powerful society to join. Hopefully, with our meeting and other things that we’re offering as we’re getting off the ground that we give people what they want, provide some value back, and hopefully start to move the needle.
Eric: I’m also wondering as we think about neuropalliative care and potentially integrating neuropalliative care into our own sites here, I just think back to your JAMA Neuro paper Benzi, so is it more of a pragmatic study, did it at three different sites, but all three different sites, if I remember correctly, did it a little bit differently. I think one site included a palliative care specialist. Another site didn’t include a palliative care specialist. How should we think about integrating neuropalliative care within our own practices?
Benzi: Yeah, I’ve been thinking about that a lot. We’re getting a project off the ground right now in collaboration with the Parkinson’s Foundation. This is a neurologist perspective. Ed and Christine can give more palliative and geriatric perspective, but the balance is really based around… We operationalized palliative care around five pillars. That was one of the big lessons, I think, from the study that you mentioned is that it didn’t matter how you did it as long as you were doing it, as long as you had a checklist and you were systematic about… What we operationalized from that study was that you were doing caregiver assessment, so asking caregivers how were they doing, asking were they overwhelmed. Checking in with patients about psychosocial issues like grief, guilt, isolation. Doing annual advanced care planning. Being systematic about checking for non-motor symptoms which are some things that always fall between the cracks. Things like depression, constipation, pain. People don’t know whether they should talk to their neurologist or primary care doctor about it. They’re often embarrassed to bring it up. Then the fifth pillar was to refer to specialist palliative care or to hospice when it was appropriate.
Benzi: That’s how we operationalized it and it’ll be interesting to see how this project develops. I think in some sites they’re going to go to more of a primary care palliative care model. Some sites it may be that there is a single nurse practitioner who is doing more of the neuropalliative care than other people. The important thing is that we’re really thinking about palliative care on a population level, kind of as a public health good rather than as an individual thing, that’s most important for somebody in crisis.
Christine: Just to build on what Benzi said, I think the building sort of depends on what resources you have. If you have resources that are present where there’s a hunger, there’s a bunch of people interested regardless of who those people are, that’s the place to start and to have them start as champions. That looks really different at lots of different places. We have some colleagues who are at a community hospital nearby and they’ve just brought in the people who are right there, who’ve cared a lot about this space, and they’re just jumping in and digging in. I don’t know that to your point that there’s a one size fits all.
Eric: Yeah, I’m just trying to think about piecing it together. Like in the dementia space, I just think back to there was a study in seven European countries, 78 nursing homes, the PACE steps to success trial. I think it was JAMA Internal Medicine again. It was a negative study. Their multi component palliative care intervention using non-specialist palliative care just didn’t do anything. I’m wondering from you’re… Does it look different for dementia than it does Parkinson’s, Christine? How should we be thinking about what… Unfortunately there’s a lot more negative studies around Alzheimer’s and related dementias.
Christine: I think that’s a really great point Eric. I’m glad you brought it up and that is that there’s this sort of surprising piece here where palliative care interventions have historically shown so much benefit in so many different settings and in so many different chronic, serious conditions. Yet, we’re not seeing that in dementia which makes me think we may have some opportunities here to better understand what the true positive palliative care components are. They probably do look different than in these other studies. The systemic review by Kieran Quinn and his colleagues that showed essentially all the benefits related to palliative care were shown pretty consistently with some exceptions for cancer and COPD and heart failure and yet didn’t show up for dementia. Physicians who were high referers to palliative care that those patients with dementia were more likely to die in the hospital and more likely to use the ED whereas all the other conditions we didn’t see that. Makes me think we have some opportunities to really learn what the secret sauce is. That palliative care for dementia is going to look just a little bit different than palliative care has historically looked for some of our other chronic, serious illnesses.
Eric: It almost highlights also the importance of palliative care for individuals with, let’s say, advanced dementia is a lot more focused on caregivers, families, nurses while it’s still important to focus on the patient and there’s plenty of palliative care needs there. The system of care is just so important.
Christine: Yeah, it gets back to what Ed was saying just a few minutes ago about the structures and how our structures really don’t lend themselves to care with family or a care of a caregiver. We really don’t have these mechanism in place by and large.
Ed: I wonder if this, I don’t know, I feel like there’s so many of the folks with dementia at a time we are identifying needs we are seeing them in crisis. I know I spend, I would say, a lot more time seeing people with dementia and their families in crisis then I do with Parkinson’s disease. I see many of them in crisis as well. I also in my clinic, we have an opportunity to be embedding practice and helping people out and making sure we put things in place before that. Whereas, I really feel like with dementia which is a huge part of my inpatient load or inpatient job, it’s not a load, forgive me. I actually, that I see people in crisis that I’m firefighting. Again, if you’re doing a ward round with 16 patients it’s very difficult to firefight effectively and so often what we do is flag things up and then we hand them back to the community. Actually how well resourceful the communities to manage these things.
Ed: I think probably there’s going to be some really, really interesting with dementia. My bet is that the hospitals is really good place to identify unmeet need because we’re seeing lots of people in one geographic space and got lots of folks, a lot of need in one place so it’s easier to maybe screen and identify. Then you’re going to need structure in the community to manage that need and the hospital is not going to be the right place to do that. I wonder maybe that’s part of what’s unique there.
Eric: I’m also wondering maybe in our last couple of minutes we can talk about lessons you’ve all learned. Especially for our audience, like key pearls you’ve learned doing neuropalliative care over the last couple years. I’m going to turn it over to start off with you Ed. As you started working with Parkinson’s folks and doing palliative Parkinson’s care, any important lessons you learned as a geriatrician on how to care for patients with neurological diseases including Parkinson’s?
Ed: Sure, thank you for inviting me to go first. That was very kind. I think the first one was having increased awareness myself and an understanding I think. I think it’s one of those areas where I really felt like my PhD submit could stand because I spent so long reading the qualitative literature. Actually maybe that’s one point, to actually read the qualitative literature. Really having that, it’s a horrible term, but that theatrical framework that’s kind of embedded and say I think your approach, I found, really affected my practice, personal practice so…
Eric: Ed, A couple examples of how?
Ed: Yes, so I’m going into a consultation with those things in the back of my mind. I really did a lot of reading about the diagnostic process and feel quite strongly about that echos right down through the course of the disease. For example, this is hardly revolutionary, the first thing I do when people come to clinic is check what they know about why they’re there and why they think they’re coming in. In PD, for example, you either get one group of folks who it’s validation. They know, they’re pretty sure they’ve got PD. There’s been a certainty on the inside. They’re coming in and thank goodness you told me this. I knew this was going on. I’ve been feeling it for years. Their response to being diagnosed is completely different to my other person who comes in having had no clue that their GP has noticed a tremor and they’ve got no idea why they’re here. The fact that before I was kind of going through the same diagnostic process for these two people with completely different needs. So, that would be one example.
Ed: The other thing that’s really challenging to myself so I would have, we all would have I’m sure, red flags in our heads for certain patients. You think this is now getting, we’ve turned the corner. We’ve got formal hallucinations, we’ve got recurrent pause, whatever the flags are that’s in our head. And challenging myself to say, have I been open in this consultation to advanced care planning. Am I picking up the cues? Am I giving off the signals that say I’m open to it? I had, I’m sorry if I’m talking too much, one really interesting thing for my research where a chap mentioned that he hadn’t had the chance to speak to someone. He was right at the end of his disease and he was still talking about his diagnostic process. He said I didn’t get a chance to speak to anyone. I wonder whose job it was to initiate the conversation. To challenge myself, I actually kind of do that as I’m in the consultation, change your body language, make sure you’re doing the right things to trigger answers.
Alex: Thank you Ed. Christine, how about from you? Lesson you’ve learned? Clinical pearls?
Christine: I loved what you brought up Ed with respect to the diagnostic process, and I would just maybe add one additional piece to that which is the whole importance of diagnostic disclosure. I think we think about diagnostic disclosure when we think about other kinds of giving bad news or we don’t think about it in the same way for dementia. For many people, dementia is more scary than the C word. Being very thoughtful and careful in the ways that we like to be in palliative care around diagnostic disclosure for people with dementia. I think it’s critically important. It can be pretty complicated and difficult especially if there’s lack of insight by the person living with dementia on their limitations.
Christine: The other thing I would say is that the importance of finding out what matters to people when they’re able to tell us what matters. It’s so critical. Often those times, they just go by, and by the time we’re actually picking the opportunity to find out what matters, it’s too late for that person to be able to speak into it when we really have to rely on their care partners.
Christine: The last thing I would say is the critical importance of anticipatory guidance that takes into account more than just the medical piece. The psychosocial piece, the environmental piece, what kind of support systems are or are not in place. Those are things that happily they’re increasing literature to guide us on but historically we haven’t really gone there to address.
Eric: That’s a great point Christine. It’s amazing the amount of frustration that always comes around finances for caregivers, our own patient’s finances, yet thinking about financed financial planning when we diagnose somebody with dementia is often sorely missed.
Christine: Sorely missed. Not addressed at all. It’s such an important issue.
Eric: How about you Benzi?
Benzi: Things I had written down, Ed and Christine covered them. I think having a good road map is so important. As a neurologist we’re trained, I think in an attempt to maintain people’s hope, to say that everybody is different. I think is helpful for us as neurologist but it’s not very helpful for individual patients. Really talking about a road map. As Christine says, talking about the road map in terms of what’s important. Can I continue to travel? It’s not just about how long. It’s also about how well as my friend and colleague Bob Holloway puts it.
Benzi: I think the last thing, kind of circling back around to come together, is really the importance of a team. That was a lesson even before the society. As I got into this field, it was very quickly apparent that there was no way that I could do everything I wanted to do by myself. That there were threats to identity and spiritual and existential issues that it was helpful to have a chaplain. There are financial issues where you need a social worker. There are things where you need good relationship with hospice. You need to know people in the nursing home world. It really takes a village to take care of somebody with a person-centered lens with dementia or really any complex serious neurological illness. I think that was a big lesson for me early on.
Eric: Let’s say you’ve convinced me. I’m really interested in neuropalliative care. How do I learn more or join the International Neuropalliative Care Society? Got it right this time.
Benzi: Glad you asked, so it’s www.inpcs.org and there’s membership there. We’re having our first meeting which we have a great agenda for November 4th through 6th. It will be a virtual meeting. It will be free. You can become a member. You can join a committee. Love to see more geriatricians and palliative care doctors and GeriPal listeners joining the club.
Eric: Awesome. I want to thank all three of you for joining us. Before we go, maybe we can come together for a little bit more Beatles. (singing)
Eric: What the heck is that song about, Alex?
Alex: I think that song is about a homeless person and their experience. How we should come together over people like this rather than what he’s saying which is just shoot me. It’s sort of in the background of the verse. That’s my interpretation. So, what do others think?
Benzi: That’s actually worth the price of admission right there. It’s always baffled me, the lyrics. I like it.
Eric: Ed, Benzi, Christine big thank you for joining us for the GeriPal Podcast. It was really wonderful to have you on. I encourage all of our listeners to check out the International Neuropalliative Care Society. We’ll have a link on our show notes on the GeriPal website. Thank you Archstone Foundation for your continued support and all of our listeners for supporting the GeriPal Podcast. Thanks everybody. Good night.