November 2010 marks the 15th anniversary of the publication of the SUPPORT Project, the largest study of end of life care ever conducted. This study that shook the medical world. SUPPORT was an ambitious effort sponsored by the Robert Wood Johnson Foundation to improve the quality of care towards the end of life in patients with serious illness. The finding that this $29 million effort had absolutely no impact on improving the quality of end of life care was stunning.
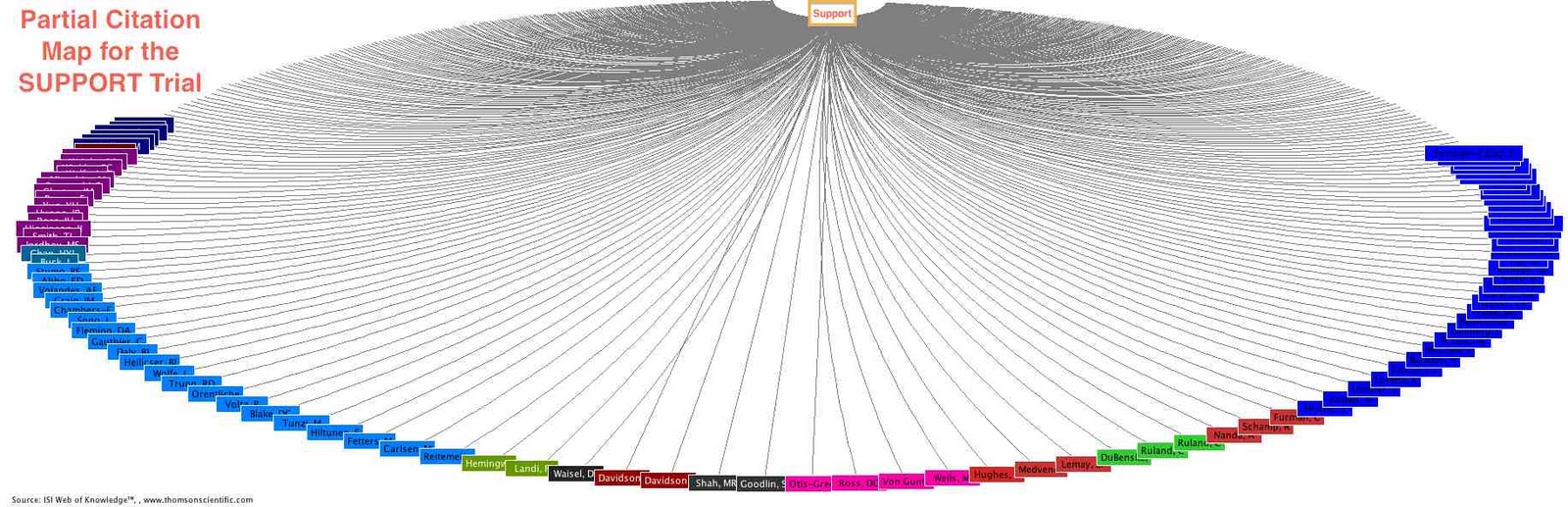
The failure of the intervention to improve end of life care and the strikingly poor quality of end of life care documented by SUPPORT led to calls for action in the lay media and by advocates of better end of life care. SUPPORT remains the most influential study of end of life care ever published, and with over 1300 citations in the peer-reviewed literature, by far the most cited.
The SUPPORT intervention study randomized over 4000 patients hospital at 5 US hospitals to usual care or the SUPPORT intervention. Patients had one of 9 index conditions, such as sepsis with organ system failure, or metastatic lung cancer, and clinical characteristics suggesting a 50% or greater 6 month mortality. Physicians of patients in the intervention received received estimates of the probability of survival over six months, estimates of the outcomes of CPR, and estimates of the probability of severe functional disability at 2 months. The intervention also provided documentation of patient and family care preferences and provided access to a nurse interventionist to facilitate communication, including helping to carry out needed communication and facilitating meetings.
The effect of this intervention? NADA. Nothing. There was no impact on each of these key outcome measures:
- Earlier writing of DNR orders
- Physicians knowledge of their patients’ preferences for CPR
- Number of days spent in an ICU before death
- Patient reports of moderate or severe pain
- Use of hospital resources
The SUPPORT project showed that the provision of prognostic information, and enhancing communication were insufficient in the 1995 care environment to improve outcomes at the end of life. The investigators suggested that “more forceful measures” may be needed. Several of the SUPPORT leaders noted that the efforts to improve end of life care were inhibited by a medical structure that made it very difficult to provide high quality end of life care and argued that improvements were unlikely without a major societal commitment to improve end of life care.
Has anything improved in the last 15 years? It seems some things have. Palliative Medicine has undergone great growth since SUPPORT. Hospital-based Palliative Medicine programs are now very common. They were practically unheard of at the time of SUPPORT. Hospice use has markedly increased.
On the other hand, the majority of patients are still enrolled in hospice less than 2 weeks before death, greatly limiting its impact. Also, I suspect that the poor quality of communication and high rates of pain documented in SUPPORT are not much better today. In addition, the delivery of Palliative Medicine into the care of the older patients with conditions such as dementia and progressive functional dependence remains minimal. Unfortunately, much of the medical world still thinks it’s necessary to choose between Palliative Medicine and life-prolonging care. Regrettably, Medicare policies continue to have an insidious role in limiting the reach of Palliative Care to many of the patients who could benefit the most.
While the negative results of SUPPORT were a great disappointment at the time, by galvanizing efforts to improve end of life care, and accelerating discussions of how to better improve care, it is has left an invaluable legacy. Beyond this, I would like to comment on two additional legacies.
First, while much focus has been placed on the unsuccessful intervention, not enough focus has been placed on the over 100 SUPPORT publications that have greatly increased our understanding of care at the end of life, and care of the seriously ill. This included a comprehensive description of the end of lifefrom the perspective of family members, prognostic tools to better understand outcomes following nontraumatic coma, and a description of seriously ill patients’ preferences for communicationabout end-of-life care decisions. There were also other findings that had broad impact on the practice of intensive care medicine. SUPPORT initiated the downfall of the Swan-Ganz catheter by showing that patients receiving this device did not have better outcomes–a finding later confirmed in randomized studies.
Finally, one legacy that deserves more mention: SUPPORT started the careers of many health outcomes researchers, and there are many of us who give SUPPORT credit for starting our careers. The SUPPORT leaders were intellectually generous, and gave junior investigators easy access to their database. Many of the high impact ancillary studies produced from SUPPORT were the author’s very first research article. Most of us given this access had little of tangible value to offer the SUPPORT investigators. All that was asked of us was rigor in our approach and an insistence on producing excellent clinical science.
At the Beth Israel Hospital, I, like virtually all General Medicine research fellows, did projects with SUPPORT under the wise tutelage of Beth Israel site leader, Russ Phillips. Russ provided us access to this invaluable resource, and the mentorship we needed to publish great research. Other SUPPORT leaders, including Joanne Lynn, Al Connors, and Joan Teno were incredibly supportive of my efforts, even though I was a junior research fellow with no experience and no track record.
The Robert Wood Johnson Foundation deserves our thanks for its vision in funding SUPPORT, supporting the dissemination of the principle results, as well the support of the many ancillary studies.
The final word, goes to Dr. Steven Schroeder, at the time president of the Robert Wood Johnson Foundation, as he noted in a 1999 editorial:
“That is the story of SUPPORT, an ambitious $29 million multi-year research project that failed to identify how to improve care at the end of life. But out of that failure came a greater understanding of the complexity of care of terminal illness. The study continues to shine a powerful light on these problems, so much so that the health sector—and growing segments of society—are starting to pay attention…..I wish that The Robert Wood Johnson Foundation and other funders could produce more such “negative” studies. To do so will require finding projects that combine salience, leadership, and rigor, and, for our part, we must be prepared to fund them adequately, even through the dissemination phase and regardless of the results. ”
by: Ken Covinsky



