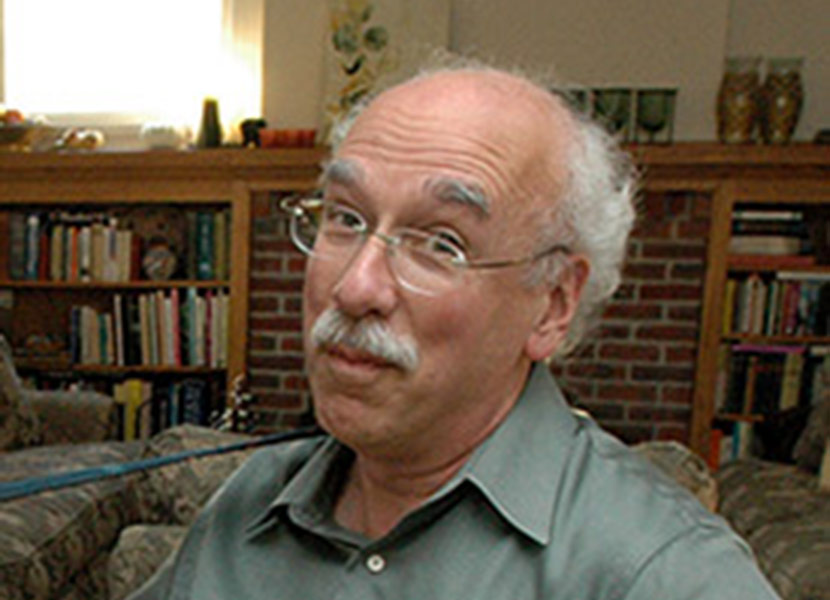
In this week’s GeriPal podcast we talk with Guy Micco, MD, a longtime bioethicists, internist, hospice physician, teacher in the UC Berkeley and UCSF Joint Medical Program, mentor, and friend.
Guy and I wrote an article recently for the journal Perspectives in Biology and Medicine about the intersection and issues between the fields of geriatrics, palliative care, and bioethics. The main thrust of the paper is that we need a workforce that is trained in the principles of all three fields to take the best care of the very sick, the very frail, and the very old.
And for those of you who listen, Guy sings a great rendition of Hello in There, by John Prine: sweet, sad, and sentimental.
Chorus:
You know that old trees just grow stronger
And old rivers grow wilder every day
Old people just grow lonesome
Waiting for someone to say, “Hello in there, Hello.”
Enjoy!
Links:
Eric: Welcome to the GeriPal podcast. This is Eric Widera.
Alex: This is Alex Smith.
Eric: And Alex, I see someone in the room with us.
Alex: We have a wonderful guest in studio today. This is Guy-. Guy Micco.
Guy: In Italiano.
Alex: Pronouncing it in Italiano. Who teaches in the joint medical program where I was a student, some two decades ago. And is a current and former mentor of mine. He is very interested in the medical humanities suffering old age and death. He has lots of experience on ethics committees, part of the subject of today’s podcast. And he works in hospice. Welcome to the GeriPal podcast.
Guy: Thank you. Thank you Alex. Thank you Eric.
Eric: So we always start off with a song, luckily, you brought your guitar. Do you have a song I guess for you and Alex to sing?
Guy: Yeah. This is by John Prine, one of my favorite American singer songwriters. He wrote it many years ago. John Prine has this uncanny wonderful ability to take the position of an other, in this case, someone old. And the song speaks I think, volumes.
Eric: Okay, let’s hear it.
Alex: Okay. [Singing]
Eric: That was lovely.
Guy: Well, lovely, I’m not sure.
Alex: Pretty good.
Eric: I would say it was lovely.
Guy: Good to know.
Alex: Your singing was great.
Eric: I do have to tell our listeners, this was a negotiation. Guy and Alex wanted to keep on singing for the rest of the podcast.
Alex: Yeah. We wanted to play for a good 20 minutes. We stripped it down, we did a 20 second, or one minute.
Guy: This song is, if we get to sing the rest of it, it becomes even clearer that the song is about the loneliness that can happen in old age. And as Bill Thomas from The Eden Alternative says, “Loneliness is one of the three poisons of nursing facilities. The others being helplessness and boredom.” This speaks to boredom also. But loneliness has to be right at the top, I think. Something medicine does very poorly with, I might add, drugs are not the antidote to loneliness.
Eric: Speaking of Bill Thomas, I was actually just listening to a podcast called the Reply All, which I highly recommend. A great podcast, more about internet stuff and technology. But strangely enough, they had one with Bill Thomas about the Eden project and a new project he’s working on. And I just thought oh my God I’m listening to this random internet podcast and Bill Thomas is on it. So we’ll include a link to that podcast in our show notes on GeriPal blog.
Guy: See old people in nursing facilities and the such are everywhere. Even on the internet.
Eric: Even on the internet. But that’s not the topic we’re going to be talking about today. What are we going to be talking about today, Alex?
Alex: Today we’re talking about bioethics, palliative care, and geriatrics.
Eric: All three of them?
Alex: All three. We have a lot of ground to cover-
Eric: Separately?
Alex: But we’ll try and keep it snappy. We’re going to talk about the intersection between them. We’re going to talk about what they have to learn from each other, and potential shortcomings of each field. And how we might address that in order to provide the best care possible for very sick, very frail, very old people.
Guy: Nice. Nice summary.
Alex: So we should mention, this discussion grows out of paper that Guy and I wrote, for Perspectives in Biology and Medicine. And we actually have a figure in there, it’s a Venn diagram.
Eric: A Venn diagram.
Alex: A Venn diagram. Look, now we’re on YouTube, we can hold it up to the camera.
Eric: Ooh.
Alex: And for those of you who are listening, we will include a picture of this in our podcast, where we draw three circles that overlap. Sort of like the Olympic rings, kind of.
Eric: Missing a couple.
Alex: With geriatrics, palliative care and clinical ethics. I think there are areas that are distinct with each field. For example, in geriatrics: care of the well elderly, successful aging, geriatrics and rooms. Palliative care, areas that are distinct: care of patients, young patients with serious congenital illness. And in clinical ethics, there are areas that are somewhat distinct, right? Prenatal testing, your confidentiality, patients endangering other patients.
There are also important areas of overlap between the fields. So between geriatrics and palliative care, for example, there’s tremendous overlap in the areas of dementia and functional outcomes. Between clinical ethics and palliative care, there’s overlap in the care of decision making for the seriously ill. And between clinical ethics and geriatrics, there’s overlap, for example, in elder abuse ,driving safety. And then all three have areas of commonality. For example, when thinking about issues of euthanasia, futility, advanced care planning, decisional capacity. And certainly those aren’t hard and fast, bright lines between the fields. But you can see that there are areas of distinction and areas of overlap between the fields.
I think that’s one part of the answer to your question, which is, really not just about the content but also might be about, what does it mean something to say that I’m a geriatrician? Or a palliative care doc, or I’m a bioethicist? And I think there’s a different answer there which has to do with a sense of professionalism. And does it mean something to have training and board certification for example, in palliative medicine? Or geriatrics? And for bioethics, I think that’s an area where there are no similar established standards in terms of required fellowship training, and board certification. And that people can call themselves bioethicists without having gone through that rigorous training.
Eric: Yeah, that’s fascinating. Because I’m on two ethics teams. I do not call myself a bioethicist, but-
Alex: You should. Maybe.
Eric: I feel like I haven’t got any, I didn’t do a fellowship in it. Am I a bioethicist?
Alex: I think you are a bioethicist. What do you think Guy?
Eric: I’m part of biology and I do some ethics.
Guy: Yeah, I haven’t seen Eric in action. But there is a core set of knowledge that supposedly one who works in the field of bioethics ought to have a lot of familiarity with, not to say perhaps mastered. But, and experience counts as well. But you’re right, Alex. There’s no board certification, there’s no coherent set. Well, The American Study of Bioethics and Humanities has tried. There are some basic ideas I think, out there that could be used for training, but no fellowship program.
It does get to the question of, what value is there to professionalism in geriatrics, palliative care, bioethics? How important is it to have these credentials? I’m not quite sure. I mean, like anything else I suppose, attitude counts a lot, at least for me. Attitude counts. But so does knowledge, attitude, knowledge. You can have had all the training under the sun and still be a poor whatever: physician, geriatrician, palliative care physician. The training is not going to help if you are lacking certain qualities, one might say virtues, of being a good doctor or a good practitioner. Because I suppose, not all palliative care team or geriatrics team or ethics team are physicians, right? So there are other people in the health care professions who partake of this.
And in any event, I do wonder what you both think being in academia now, training young palliative care physicians, young geriatricians, to be probably helping budding bioethicists become bioethicists. How much of the training involves values, attitudes, virtues? And how much is aimed at purely the, what might be called the didactic formal knowledge based stuff? That I’m sort of demeaning a little bit, but not totally. I mean, it’s very important to have a knowledge base. But the others I think, maybe are more important.
And I’ll say one more thing before I go on way too long. That is that, my view is that someone who is virtuous has the right attitude in medicine. If they don’t have the knowledge, they will find the knowledge necessary to be good at what they’re doing. Because that’s part of being a virtuous whatever. You want to have the knowledge base. And if you don’t have it, you ask, get help.
Eric: Yeah. Well, I think it’s a lot easier to train people on knowledge and procedural skills. We just had Wendy Anderson on our last podcast and we asked her the question of, can you teach or train people on empathy and communication? Short answer, she thought, yes. But the similar thing with virtues, can we train or teach people specific sets of virtue, or to be virtuous?
Guy: Well, this is a two or 3,000 year old question. And I think you can promote virtuous behavior through example. You can promote it by supporting people who display such virtues. It needs to be practiced, sort of an Aristotelian idea. You have to practice and continue to work in this realm of virtue, or else it can go away. And if there’s a hidden curriculum that the learning by example bit that is not virtuous, then people learn the opposite.
Eric: And just for my non bioethical mind, when we say virtuous, what do we mean by that?
Guy: Well, I would say there are certain virtues that lead to, or important for being a good physician. So virtue would be wanting to do good for one’s patient. So the virtue of beneficence. The virtue of want to, I mean, to use the classic bioethical words, the virtue of wanting to support someone’s autonomy, to have control over their own bodies and minds. The virtue of being present, wanting to support people by your presence, by listening. The virtue of constancy, being available to your patients. How much availability is tough to know, and you’re balancing various other responsibilities as well. Not just to your patients but to yourself, your family, your community.
But having in mind that doing good-that one as a physician wants to do good for one’s patients. Having that foremost in mind I think, leads to the understanding that knowledge is incredibly important. And being able to do the procedure properly is incredibly important. So it’s the first on my list of things to support and promote.
Alex: My favorite virtue is the virtue of caring, which is very related. Caring about your patients. A lot of this comes actually from nursing and feminist ethics, that the real outrage over the atrocities of the Nazi physicians came not because they violated any of the classic ethical principles, but because they just did not exhibit fundamental caring that one should have for another human being. And that is probably the core, one of the most core virtues of the good doctor.
The other one that I remember you talking about in medical school is aequanimitas. Could you say something about that?
Guy: Oh, aequanimitas.
Eric: Wait, what does that mean?
Alex: [Aequan 00:14:49], horse.
Eric: Something about a horse.
Guy: Yeah. Something about a horse. I suppose it’s a calmness in the storm. But aequanimitas was the name of a famous speech that Osler gave at a commencement, probably around 1900. In which he promoted the view that physicians need to curtail, to hold back, to control their emotional lives in dealing with patients. And that one way to put that is you don’t cry into the wound, it doesn’t do anyone any good. And in fact, it leads to poor outcomes, because your emotions can’t be trusted.
So he’s been taken seriously for a very long time in this issue, and it may go back to Hippocratic times. But there are people now writing about how that’s too intellectual a point of view, it’s impossible to really control one’s emotions to the extent he was asking, being the promontory against the storm, or against the tides that are wearing away the side of the cliff. It’s impossible actually, to be that way. But in trying to be that way, one is perhaps, too cool in relations with patients. And we’re asking, I think now, of our students and ourselves, to be a little warmer, to be more empathic in the sense of showing some feelings. Not being cold and aloof from the feelings of others, but letting them in. And then of course, they’re going to affect us. And what we do with that is, it can be very difficult how to handle one’s emotions.
Eric: I was just talking to one of our medical students and resident teams after a really tough family meeting. And the question was, how do you do this without crying? And my response was, how do you do this with …
Alex: And not cry.
Eric: Yeah. Why not cry? You just witnessed suffering on a grand scale in this family meeting. Why not cry? And if you’re not feeling these emotions of sadness when you’re in this with a suffering, something is wrong if you feel like you’re not gonna cry.
Alex: It’s interesting. I wrote a paper back in residency with a medical student, who surveyed interns, very stressed out right time of year. Or a year in their lives. And third year medical students, another stressed out time of year, at two medical schools and residency programs. About crying, which he’d defined as a visible trickling tears down the face.
Eric: That’s very objective.
Alex: Very objective.
Eric: Did you quantify how many milliliters? Does it count?
Alex: Just as long as you got to the tears trickling down. It could be welling up, that didn’t count.
Eric: Okay. It couldn’t be sweat either?
Alex: No, it had to be tears coming down. And he found that, we talked about the hidden curriculum before, that many medicals … So first of all, he found that two-thirds of medical students and residents had cried in healthcare settings out of stress and out of sadness. And they felt like it was more okay, it was more acceptable to cry out of sadness, than out of stress. As long as it didn’t reverse the patient-physician dynamic.
The other thing he talked about is, when medical students and interns reported that when they saw attending physicians cry, that the attendings would run away, compose themselves and then come back. There was no discussion of it. Much as you just had discussion of it right now. And then it was a missed opportunity and that there may be this hidden curriculum that we develop people. We sort of strip them of some of that outward display of emotion, which may in fact lead to stripping them of some of that inward feeling of emotion? Which may make them less empathetic over time rather than more.
I think there’s a different sense of aequanimitas that I’ve taken. When you see a physician or a clinician, when there seems to just be chaos whirling around them, and they’re able to maintain their calm and their perspective, and choose the right course, right? That’s the way I see it. The virtue in its best light. I do understand how there also can be this overly cool aspect to it, but I think there is something there.
Eric: For any of these, right? There’s a balancing. You can go too far. I agree. I think when I see those physicians who not only don’t do well with chaos, but bring chaos into the room. Things go incredibly bad. But we also don’t want to take out that emotional part of what it means to be a physician. So finding that middle ground, how do you do that?
Guy: Yeah. Well, points well-taken. Equanimity and calm are virtues that I think, are to be promoted. How do you do that? Not by being an intellectual cool as a cucumber kind of a person who eschews the emotional and pushes away the tears. But maybe by having a meditation practice or a spiritual practice of some sort that grounds oneself, and helps one accept suffering, maybe that … In fact, I think that would help. But to merely model the coolness of the attending, who in the long white coat has total composure in the face of intense suffering. I just think that’s the wrong model, at least as you say. It ought to be talked about.
Eric: And maybe some mindfulness just to acknowledge that this is how I’m feeling right now. And it’s okay. And what I want to do about it. I’m just reflecting on a story I heard yesterday, where there was a family meeting that felt very chaotic. And the palliative care team just acknowledged the chaos. And I thought that was-
Alex: In the moment?
Eric: In the moment.
Alex: In the moment.
Eric: In the moment. And I wasn’t there, I just heard about it. But I thought it was, that was a brilliant, mindful maneuver to just acknowledge what they were feeling in the room-
Guy: With the family of that patient.
Eric: And everybody in the room. And I think what we worry about is, it’s gonna cause more chaos. It’s kind of like the old thought with suicide, don’t bring up suicide else like, people would think, “Oh my God. That’s an option.” And acknowledging our emotions or the emotion in the room, or the chaos in the room, will bring more chaos. And it usually doesn’t.
Guy: No. Mindful chaos. I mean, being aware and pointing out the obvious to everyone sometimes can be a relief. And allow people to move on to the next or to what needs to be done. Equanimity cuts two ways. Like you said, Alex, I think. On the one hand, if it comes at the price of tamping down one’s emotions into I’d like to say, the nucleus ambiguous, somewhere in the base of the brain. Just push all the emotion down in there.Sometime in the future, it’s gonna pop up in some hydraulic fashion and cause trouble. So, not suppressing or not repressing. Maybe it is suppressing at times, holding on when it’s inappropriate to show certain strong emotions making … Whenever an emotion is about me, probably one ought to be cautious about letting that go. And when it has to do with the total situation and the suffering of others, I think it’s appropriate for instance, to cry. I don’t see a problem with that.
Alex: Well.
Guy: Where would you like to go next?
Alex: That was very interesting.
Eric: All right. We took a little bit of a tangent, but I want to go back to, so you have this paper that you published on this intersection between geriatrics, palliative and bioethics. And I think they’re really interesting. Because I’ve seen papers around the intersection between geriatrics and palliative care, and we’ve talked a lot about that.
But adding a component of bioethics I think, is really interesting. And especially when we’re using specialists like bioethicists or ethics teams. Can you give me, and I think you had an example in your paper, of how this would work in real life?
Alex: Right, what are we asking of ethics teams? I wonder, we could use the example from paper, or do you have an example from your experience that illustrates-
Guy: A good one or a bad one?
Alex: I think probably a bad one is more interesting.
Guy: A bad one. Yeah, I have several bad ones. Physicians I think, in general, this is a stereotype. And I do believe it’s changing for the better. But in my era of training, physicians were just trying to move from being the Godhead, the head of the team. In fact, was there a team? Physician was the end-all be-all, the decision maker. And the patients, the virtuous patient would just attend to what the physician had to say and follow their directions, right?
The virtuous physician was the beneficent God who is always going to do what was thought to be in the best interest of the patient. You could trust that, physician was interested in the best interests of the patient. But it didn’t take into account what the patient thought was in their best interest, particularly. Because what did they know? Did they go to medical school? No.
Alex: No.
Guy: Okay. So enough said about that. The physician was the king of the realm. And when I was in training, things were changing. It was the era of the beginnings of patient autonomy. The death knells were being told for physician, that the idea that the physician was at the top of the heap here, and the pedestal effect was going away. But still the lingering part of that is that physicians generally, another broad brush here, don’t like to be told what to do. So if an ethics committee is called to meet to talk about what to do, and has ideas presented that are different from what the physician has, as the primary care physician in the old days, but now the hospitalist or the intensivist. What they think is the right course, there’s going to be potentially some trouble.
At one ethics committee meeting, I recall, we had a wonderful discussion, open discussion with family, patients, surrogates, nurses, physicians, consultants. The primary care physician at the end stood up and says, “Well, I’m not going to do that.” And walked out. End of that story. We don’t expect the physician to do what’s …
Eric: Recommended.
Guy: Ya Recommendations are recommendations, but they’re taken as directives sometimes. And that’s not what we want to say, but it would be nice if they were considered.
Alex: Mm-hmm (affirmative). We critique bioethics, part of the article is the critique of each field and what it has to learn from the other. And we’ve noticed on our ethics committees that we’ve frequently moved to one of our first recommendations, being a consultant palliative care committee, or a palliative care consult rather. I think a big part of that is that the ethics committees themselves are not well designed to form relationships with patients and their families, and that there are some bioethics consultants who do this and do it well. But generally, the ethics committees, it’s almost more like a hearing on the subject, unfortunately. It can be like that. Which is more like cold and dispassionate, getting back to our discussion of aequanimitas.
Eric: Rational.
Alex: Right, rational. Weighing of different factors, different issues, ethical issues at stake. Whereas palliative care, and I’m speaking in a room full of palliative care trained physicians. We form a relationship first and we view that as an essential first step in negotiating these complex often difficult, highly emotional topics. And that there has not been enough value placed on the forming of a relationship in bioethics. And there’s something to be learned from palliative care.
Guy: I couldn’t agree more. Where’d you learn that? That’s very good.
Alex: From you!
Guy: Oh, that’s very good. It’s the reason why I still, this almost sounds like the crotchety old fart physician complaining about how it used to be, but it used to be … The best of what it used to be was, a primary care physician who knew the patient, followed them into the hospital into the ICU, cared for them through crisis. Maybe two, three, I think COPD patients. Three, four or five admissions to the hospital for acute exacerbations of COPD. Come back, follow them in the outpatient clinic or in their office, the primary care physician’s office. Knows the family, knows the spouse. Have discussions with them about what’s been happening.
Another crisis back into the hospital, discussing issues. Getting to know them well, having a relationship. And then when things hit the fan, it’s infinitely easier than having a consultant come in. And the anecdote, I know you know, Alex, that I’ve told before, is, when I first did palliative care at a community hospital. A physician, whom I knew, an intensivist, came up to me, saw me in the hall. And says, “Oh, I hear you’re part of a palliative care team. That’s great. I of course, don’t need any help with symptom control. But some of these patients, you got to get these families on board. You really do.”
So we have to find a way to integrate palliative care and bioethics and intensive care knowledge and procedural acumen together. Now maybe that means having members of the palliative care team in the ICU seeing patients from the very get-go. Maybe it’s someone with ethics background also doing rounds in the ICU daily, not weekly. Not ad-hoc coming in you know as the, please God help us get this family on board, this patient’s dying. But actually, having input on rounds on a daily basis from the time the patient enters the ICU. This is in the absence of having a primary care doctor who hopefully would have had all of those abilities wrapped into one, plus the knowledge of the patient.
Eric: Alright so. But like in reality world, thinking about like, so for every ICU, are we going to have a geriatrician, a palliative care doctor, a bioethicists, well-trained by clinicians in multiple different specialties, seeing all of these patients? When there will never be enough geriatricians, palliative care doctors and bioethicists.
Guy: Well, we want to infuse, right. I think it would be optimal to have people who have all these trainings on an ICU team. But no, you’re gonna have to have some infusion of geriatricsization palliative care …
Alex: Palliatization? Palliative-
Guy: Pallia..?
Alex: Palliation? No.
Guy: No.
Eric: Primary palliative care.
Guy: We have to inculcate these values and skills, and every doctor should probably have these skills and abilities and virtuous attitudes. But there are some special people who could add something to an intensive care unit team on rounds. I think for instance, maybe a chaplain. A good chaplain who’s ecumenical and has communication skills that transcend in some good way. Or a social worker. Or maybe it’s a palliative care physician or, I don’t know. Someone who brings this special something about communication and relationships.
Eric: Mm-hmm (affirmative). All right. I got another question for you, Alex. Because you mentioned, on ethics committees you often, first recommendation is for a palliative care consult. Where does geriatrics fit in? Does it?
Alex: Well, it does. But it depends on the setting. And often the ethics consults are about life and death sorta issues. I think that geriatrics fits in more often in the outpatient setting. And more often when we’re thinking about what sort of care could have come before for very old, very sick, very frail, older adults that would set them up in advance. And oftentimes for example, that’s care that takes place in nursing homes, or home-based care, where we want teams to be infused, to use Guy’s word, with principles from geriatrics and palliative care and bioethics.And that geriatrics has a tremendous amount to contribute in terms of understanding what patient’s goals are. And you might say, “Well, that’s a principle from palliative care.” But I think in geriatrics, there’s a strong understanding, a deep-seeded understanding that people value function often above other factors. And that in most of medical school we’re taught about how to preserve quality of life.But in fact, in geriatrics, quite a bit what we talked about, is how to maintain somebody’s function. And that doesn’t mean necessarily preventing disability, but a lot of time helping people to accommodate, to live successfully in the community as independently as possible for as long as possible. Providing support for them to live in the community, making it possible for them to receive treatment in the community rather than coming into the hospital into the intensive care unit.
And if we can infuse care teams with that sort of, geriatricize them, then we may actually prevent some of the head-to-head conflict that we see between providers who have very strong opinions about what are we doing here, we’re flogging this patient. And patients and families on the other hand.
Eric: Okay. Critique.
Alex: Critique of palliative care. We already mentioned this to some extent, that people who go into palliative care, especially young you know we’re just finishing the summer now and a lot of young trainees, fellows in palliative care are starting. And part of what motivates young trainees to go into palliative care is their experience in medical school and residency. Where they’ve seen suffering at the end of life and what they perceive as people being kept alive with poor quality of life. And there’s a zeal that they develop to try and prevent some of this, and that zeal can sometimes be blinding. And blind them to some of the nuance and the subtlety, and the ability to emphasize and take that step into the patient’s shoes, into the family’s shoes, to see things from their perspective.
Because we shouldn’t be going into palliative care because we feel strongly that we have to get patients to stop being flogged, or torturing them at the end of life. We should go into palliative care because we genuinely want to help match the treatments that patients receive to their goals. And that often when patients have an informed understanding about the risks and benefits and potential harms, they will more often choose paths that are less acutely intensive than what they might have done in the usual care pathway.
Guy: But that’s not the reason we’re doing that.
Alex: That is not the reason we’re doing it, yeah.
Eric: I think of it a little bit differently is, I actually think it’s fine if people actually decided to go into palliative care, because they feel that way. Because I think that’s very common for new fellows to feel that way. And I think part of our training should be …
Alex: To help that, appreciate that nuance.
Eric: To help that appreciate that a good death is not a helpful terminology. What we think is a good death or a good near-end of life is very different. But because I do feel like this is the number one thing in the first three to six months of fellowship that we sometimes have to get over.
Alex: Yeah, agree. We get them into the field this way. But then we need to retrain them, get them to-
Eric: Yeah. And it’s to acknowledge, I still feel that way sometimes. I still feel like, “Oh, my God. Why are you doing this?” And just acknowledge and be mindful of that feeling and decide what do I want to do with it. And maybe it’s actually just tell people, why are we doing this? This is something I’d strongly recommend not doing, and these are the reasons why. Rather than be it like this implicit feeling like, “Oh my God. Why?”
Guy: Well, that’s good.
Eric: Well, we are approaching the end of our podcast. There’s so much more we could talk about. But how about we actually end with a little bit of song. Before we do that, I just want to thank you Guy for coming here and joining us in the studio.
Alex: Thank you Guy. I really appreciate you coming over here.
Guy: Thank you. Thank you Eric. Thank you Alex.
Eric: Ok, let’s do a little bit more.
Guy & Alex: [Singing].
Eric: Well Guy, I just want to thank you for joining us again today. And thank you all of our listeners. If you have a moment, please take a second and just rate us on your podcasting software, whether it be iTunes, Stitcher, or-
Guy: Not on the singing. We’re not talking about the singing.
Eric: Not on the singing.
Alex: The singing was great. That was great Guy. Thank you.
Eric: And we look forward to having you on our podcast next week.
Eric: Thank you very everyone.
Alex: Thanks folks. Bye.
Guy: Well, I muffed one line.
Alex: I thought it was great!



