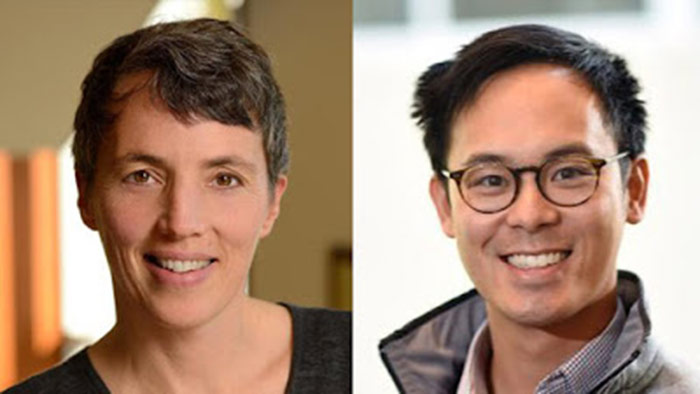
Ken Covinsky previously posted on GeriPal a while back about the dangers of hospitalization in older adults. Ken notes in that post that hospitalization is a vulnerable period leading to major new disability for many older adults. More recently, Ken, GeriPal contributor Bree Johnston, and honorary GeriPal member Edgar Pierluissi authored a terrific article about hospital-associated disability in one of those pre-blogging era, old-fashioned periodicals…JAMA.
I’m not going to be able to sum up this meaty piece of scholarship in this post. Let me say only that if you care for hospitalized older adults, and can only read one article that changes for the better how you care for them, this would be that article. Let me relay some of the disruptive perspectives offered:
- Move over traditional geriatric syndromes, and make way for the newcomer: hospital-associated disability should be considered a geriatric syndrome (the “hospital disability syndrome”). Hospital-associated disability shares hallmark features with the well-established geriatric syndromes, such as falls, delirium, and incontinence. The etiology of hospital-associated disability is nearly always multifactorial. These syndromes occur in older adults who have accumulated impairments across multiple domains, and are vulnerable to the stress of an acute illness or hospitalization.
- Stop using “the one-point restraint.” By that they mean a urinary catheter (Foley). Much of what is routine about hospitalization impairs older adults ability to recover and promotes additional functional decline. Some key examples: bed rest to prevent falls (immobility leading to loss of function), diphenhydramine to help the patient sleep (delirium leading to loss of function), and a urinary catheter (restraint leading to immobility leading to loss of function). They suggest that the benefits of accurate measurement of urinary output with a catheter are outweighed by the risks of infection and immobility in the elderly. Next time you admit that 80 year old with a CHF exacerbation, rely on daily weights rather than putting in a catheter. Help them walk to the scale.
- Let them eat food, and food with taste. Have you ever had a no-salt, low carb, fat free meal? How about being offered that for breakfast, lunch, and dinner for days on end? No wonder nutritional status drops quickly with hospitalization, and that doesn’t even count the nothing by mouth (NPO) order that older adults are often slapped with until the speech and swallow folks can assess them (on hospital day 3).
- “Discharge rounds” should be renamed “going home rounds.” “Discharge” is utilization focused, and aligns with the hospital’s financial interests, as they are generally paid a set amount of money for a given admitting diagnosis. The shorter the hospitalization, the greater the profit for the hospital. “Going home rounds,” in contrast, is patient centered, and recognizes that return home from hospitalization is an important transition that requires proper planning and support.
- Mortality is high for older adults with hospital-associated disability. As high as 40% at one year! Palliative care should be a key part of the care plan. So what is palliative care for disabled elders? Yes, pain is mentioned, but so are several features that certainly weren’t on the palliative care boards when I took them last year: motorized scooters to make getting around easier; home modifications such as support bars and a shower chair to promote independence at home; and paratransit services to facilitate independence outside of the home. These features support disabled older adults’ dignity at a vulnerable time, in what may their last months of life. Sounds like palliative care to me.
by: Alex Smith