This week we have Lee Lindquist with us on the GeriPal podcast to talk about planning for the “4th quarter” of life. Dr. Lindquist is a geriatrician and chief of geriatrics at Northwestern Memorial Hospital and Northwestern University Feinberg School of Medicine in Chicago.
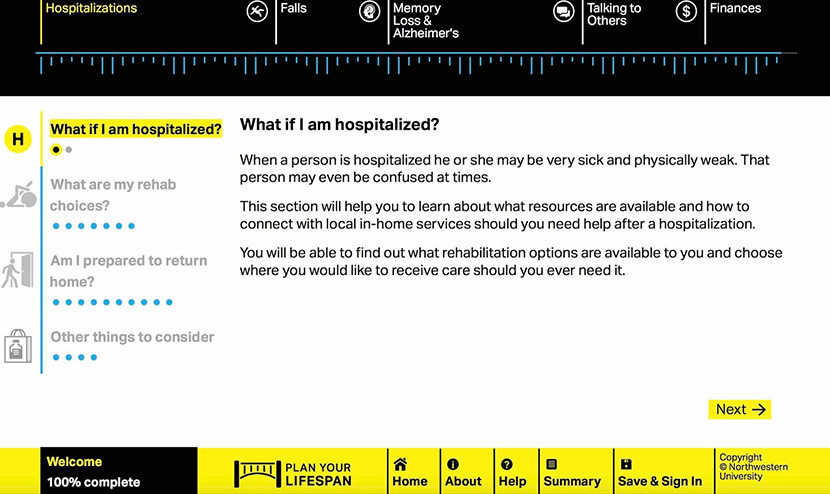
Dr. Lindquist developed a free to use website called PlanYourLifespan.org to help older adults create strategies for dealing with health crises, such as hospitalization, a serious fall, and dementia. No this is not just end-of-life issues. Using the website, older adults can think about what services they may need in the last 10 or 15 years of their lives, what choices they can make now, and how to access these services when needed.
So give it a listen and comment below on what you think should be addressed in the last quarter of life. Below is also the link to her randomized control study showing increased understanding of posthospitalization and home services compared to the control group.
Eric : Welcome to the GeriPal Podcast. This is Eric Widera.
Alex : This is Alex Smith.
Ken : This is Ken Covinsky .
Eric : And Alex, who is our special guest today?
Alex : Today we have Lee Lindquist who is chief of the division of geriatrics at the Northwestern University Feinberg School of Medicine. Welcome to the GeriPal Podcast, Lee.
Lee : Thank you very much!
Eric : We always start off these podcasts with a song request. Do you have a song?
Lee : I do have a song. My song is Go Cubs Go!
Eric : Oh no!
Alex : Yes! Yes!
Lee : We’re in Chicago, and it’s the awesomest song ever!
Eric : That’s why Ken is here!
Lee : [inaudible 00:00:35] huge cubs fan here in Chicago. (singing)
Ken : Aw, that was good.
Lee : Yay!
Alex : That was food for Ken and Lee’s soul. What’s the deal with this song, Lee? Something about a cub? Is that a bear?
Lee : So this song is the best song in Chicago, called Go Cubs Go. It actually is very fitting for our conversation today because, you know the Cubs were on such a drought getting the World Series up until 2016.
Alex : Oh, did they win?
Lee : It’s like every day you’re planning for something to happen, and it did. So we’ve got a great team, and it’s the best.
Eric : Ken, I don’t think you’ve ever mentioned the Cubs winning before.
Ken : I never talked about this did I?
Eric : Never, never.
Ken : 2018 is our year again.
Alex : So you plan for the worst, and then who knows? Maybe something good will happen?
Lee : That’s right. Everyone’s planning with new pitching, getting our bullpen stronger. But that’s something that I think among my seniors, because as a geriatrician I see patients in my outpatient clinic in geriatrics and we’re trying to always have our seniors plan ahead for health crises. That’s kind of how I came up with my research project Plan Your Lifespan.
Alex : Awesome. So tell us more about the Plan Your Lifespan project. Starting to get in to where it started, and what the motivations were. Can you say more about that?
Lee : Yeah, totally. Whenever I see patients, often times … I love my patients … and what happens is, I’ll sometimes get a phone call from a family member saying, “oh my god, so-and-so fell, they got hospitalized.” Or you know, “I went to visit my grandmother, or my mom, and her memory is getting shot, and she’s all over the place. What am I supposed to do?” This where we see patients in crisis mode, and then the families have to run around and try to figure out everything to do, whether it’s hiring a caregiver, or finding a good skilled nursing facility. And that’s where I would get a lot of phone calls, is “oh my god, so-and-so went into crisis mode.”
It’s kind of a given that your favorite senior is going to either be hospitalized, or you know, experience a health crisis, whether it be worsening Alzheimer’s or a fall. That’s really going to just change their entire outlook, like their lifestyle. It’s going to really impact their ability to age in place. So instead of having this conversation … and usually the senior gets left out of this conversation … I figured lets give the seniors a voice, and let’s tell them what choices they can make now, and plan ahead for the future. So this is not for planning for end of life. I call it planning for your ten to twenty years before you die, which is kind of like the … some people call it the fourth quarter of life. It’s where you become more disabled or you have problems with disability and more needs.
Ken : But Lee, you said something interesting there, you actually used the phrase “it’s kind of a given.” Is it really? Because it seems a lot of the health gurus and self-help gurus … you know, if you listen to them, they kind of sell a vision of aging where this isn’t a given. If you do all the right things, you can prevent this stage of life. So is that true?
Lee : You know what I see a lot with my patients is that they think … and I love the ePrognosis stuff that you guys are doing out there … but what I see a lot of my time with my patients is that they think they’re going to live with full vitality, and then all of a sudden just die in their sleep suddenly. Then they’ll never need any assistance or anything. We know that not to be true. Nobody is that lucky to die in their sleep and never have any problems before they die. I’m sure there’s a few, but that’s not par for the course. I think if we can extend people living longer and feeling better, I think that’s definitely something we should all be going for as a successful aging piece. But I think down the road, people that really do need the plan for accidents or crises that happen, just so that seniors can have a voice.
Eric : What you did is you created a website, and it’s planyourlifespan.org.
Lee : Yes.
Eric : Tell me, how did you think about designing that website, putting it together, what was your inspiration? What are you hoping older adults will do with it?
Lee : We got a nice size grant from PCORI, which is Patient Centered Outcomes Research Institute. They funded us to bring together a lot of seniors and social workers and family caregivers and Triple-A area agencies on aging. So we brought a lot of community partners and seniors to the table and asked them, “what do you think is going to impact your ability to age in place?” From that we identified three main crises, which is hospitalizations, falls, and Alzheimer’s dementia.
From there, we started saying, “okay, what information do you need to know now, in order to make an informed decision.” How fantastic would it be for a senior to say, “okay, down the road, I might be hospitalized, and I might need a caregiver to come to my house, or I might need to get to a skilled nursing facility. Which ones are in my area that I would be willing to go to in case of a crises?”
This actually … planyourlifespan.org allows people to make decisions and understand what their needs will be in a crises, before the crisis even happens. How sweet would it be for somebody to say, “you know what? If I ever do get hospitalized, this is what I want for my care after I get hospitalized.” What’s great is that with this website, it’s publicly available nationwide. You can actually enter in your zip code and find out what services are available in your area, or what are the closest skilled nursing facilities, or where can I find meals on wheels, or my Triple-A, my area agency on aging. It’ll come up, and you can make choices. Then you can actually print it up, or you can email it.
When we did it, we actually found that a lot of people were kind of hesitant to talk to their loved ones about this. I’m sure you see that a lot with palliative care, or with hospice and making decisions. We actually had it so you could actually email it to your loved ones. Decisions like if I do need extra support in a home, or I’m not able to live alone, I’d love to have a family member … I’ll move in with the family member, or I’d be willing to have somebody come to my home. One of the great stories that we had was that people … there was a couple people that said, “well, I’m going to move in with my son, Ken.” They said when we talked to the son, the son was like, “oh, I didn’t know this was going to happen, I didn’t know they were interested in moving in with me.”
It really stimulates conversations. We actually added on two extra parts, which were on communication and finances.
Eric : How much does the website cost to use?
Lee : It’s free! What can you say about that?
Ken : Good job Lee.
Lee : It’s free to use.
Ken : Lee, I think the work you’re doing is an amazing service. It struck me as I’ve been thinking about your work that there’s been decades of discussion about advanced care planning and planning for the future, but it’s tended to focus on end of life planning. This seems to be such an elephant in the room, the kinds of things you’re talking about. Planning for the stage of life where you’re maybe physically and cognitively disabled is something that we’ve never talked about. Why do you think there’s such reluctance to talk about this. I think you’ve done the first step of making this information available, but it seems there’s a huge cultural reluctance in society to acknowledge this phase of life.
Lee : You’re absolutely right. We actually did the next step where we asked people, “why aren’t you planning for this, why are you resistant to planning for this?” A lot of people fear the loss of independence. We even nicknamed it FOIL for “Fear Of Independence Lost.”
People, when they start planning for this, they think it implies they’re going to lose their independence faster. Which is not the case. Just to touch on that advanced care planning part, we see sometimes that people say, “well, I’ve already got my will, my power of attorney, my POLST form, I’m done.” That’s not the case.
Alex : So maybe you can tell us a little bit more about the specific trial that you published in the Journal of Hospital Medicine. We’ll have a link to it on our website … Helping Seniors Plan for Post-Hospital Discharge Needs Before a Hospitalization Occurs.
Lee : If you think about it, so many times when a senior gets hospitalized, they’re just laying in bed, and they can’t really make decisions. Then the family caregiver has to run around, and sometimes they have full time jobs. They have to run around and look at different skilled nursing facilities, or arrange things for a senior to get home. It really is a problem, because the senior doesn’t have a voice in it, and then the caregiver is just making their best choices. So what we ended up doing is we did a randomized control trial where we randomized about 400 people, seniors, who were living in the community. We randomized them to either doing the planyourlifespan.org, or to a control website. People that actually did the website found it to be very beneficial to them. It helped them in making decisions, helped them planning, and also helped their understanding of what they might need down the road.
It’s kind of a way of empowering your patients, empowering your seniors to know more about what they need down the road before it actually happens, and to give them a voice.
Eric : What kind of information did the website teach these people in particular? You mentioned hospitalization-
Lee : It taught them … oh my god … it’s so cool, because it actually teaches you a lot about the information that we doctors use, or we nurses or nurse practitioners. Like, a SNF. We use that term all the time. People don’t really know what that means, it’s a skilled nursing facility. We actually go through some of the lingo, what actually are the differences in physical therapy that people can get in their home. What things they should be getting in their home in order to go home. Things that people don’t even think about, like where am I going to get my meds, how do I get my food, how do I get my medications delivered. It makes people critically think about what they’ll need down the road. How sweet would it be for a person to come in to the hospital and the caregiver or the family member would already know what they need afterwards. It’s a great means of having this discussion.
What’s fascinating too is that there’s so many health providers out there that haven’t talked to their own parents about what they would want in the future. We’ve had discussions about end-of-life, tubes, all that stuff, but we really haven’t had a lot of discussions even with our own parents about if something happens to you, what do you want to have done? Or what should we do? It’s kind of interesting to hear health providers even talking about it with their own parents.
Ken : I think what I find interesting, Lee, is that I’ve had the same experience in my clinic as you. When you practice geriatrics you see this full range of function. There’s something remarkable about a 90 year old who is fully cognitively alert. Walks up our steep hill to the clinic to get in. When you see patients long enough, you realize that, that person who is blessed to be so functional at 90, they become 95 one day, and they have all the problems of aging. There’s not a lot of escape from this. Those that are fortunate, it’s not that it never happens, it’s that it happens later. What practical advice do you have for the patients thinking about this? What kinds of things do you recommend a patient do now to start planning.
Lee : In my practice, when I’m talking to patients, we all have end of life … if something happens to you down the road, what would you like to have done. When people have already said, “I’m going to have … I already picked out my power of attorney.” I usually ask the next step, “what about the 20 or 30 years beforehand. Or five or 10 years beforehand. Have you thought what you might need if something happens.” It’s a way of getting people to think about these things, and to have general conversations with family members. Then also to pin points so that there is a plan A and you’ve got a plan B for if something happens.
It’s a way of giving people empowerment and the voice in their future, but also decreasing burden on their family members, so that they have a knowing ahead of time of what they might need to take care of their beloved senior.
Alex : I have a couple of questions about this analogy to advanced care planning, and how far it extends. A couple of thoughts. First is, in advanced care planning … a couple of the insights from Rebecca Sudore have been that you can’t plan for everything. There will be circumstances that are unforeseen, so the best you can do is plan in advance to prepare people for those unexpected moments where you have to make a decision that you weren’t able to completely plan for previously. So the conversation becomes one of the most important parts of the preparation steps.
The other thing is talking about leeway, and giving surrogates who are making these decisions when patients are unable to, some degree of leeway, of flexibility around the preferences that have been established in advanced. Or not, if those preferences are fairly strongly held, deeply believed, and fixed.
I’m wondering whether those aspects have been incorporated into this … I don’t know what call it, the domain. The pre … the long term advanced care planning, or whatever-
Lee : We actually call it fourth-quarter planning.
Alex : Fourth-quarter planning.
Lee : Fourth quarter planning is what we’ve been nicknaming it. That came from our seniors and our older adult patients that were participating in the study. Nobody liked calling it pre-death based, but going after it as a fourth-quarter … because it’s just the next part of your life … is kind of the moniker that we’ve been using. There is leeway, even with the website. You can keep going back in as many times as you want. You can change things. You can save things underneath your name on a secure server, or underneath a code. You can keep going back in and making changes.
But I do agree with you that it is the conversation that’s important. What do you want to do before you die for the ten to twenty years beforehand. Not everyone can be prepared for everything, but we can be prepared for what you might need, or if somebody’s needs increase. The biggest question I’ve seen is, do you want to stay in your own home as long as possible, and have people come and see you or help you out. Or do you want to move in with somebody. That’s been the biggest path in the road.
Eric : How realistic are individuals when they’re thinking about the future? For instance, yeah, I would love to have 24-hour caregivers at my home, that sounds great, I’m going to put that down, without realizing it’s going to cost … like in San Francisco … over $20,000 a month for that type of care. It’s unpractical for 99.9% of the population. When they’re filling this out for you, do you see the same thing, where there may not be an understanding of cost?
Lee : We added on a section on finances, because there was a lot of … we did qualitative interviews with people, and a lot of people felt that Medicare would pay for everything, Which we know not to be true. We have things in the finance section of, listen, this is what Medicare is usually paying for, this is what long-term care insurance might pay for, and this is what you’ll have to do out of pocket. I think even having that conversation and talking about, “this would be my goal, would be to be in Hawaii for the rest of my life and have caregivers in there.” Sure, that sounds sweet, but it might not be practical for some people. Having that conversation, deep down, what is feasible and what’s not, and knowing that it might change, I think is the communication. You’re spot on, on that.
Ken : Lee, how often is it appreciated by older persons and their families the extent or magnitude of effort that will be involved? I can imagine on one level, mother and daughter might say mother wants to move in with her daughter, but is it recognized that it’s not just moving in, sometimes it’s like, mother’s going to need help getting out of bed, and getting out of a chair. Or mom might have cognitive problems and might need continuous supervision. How much into the nitty-gritty do you get in terms of what exactly is involved?
Lee : On the website, the planyourlifespan.org website, we get down to who would take care of your dog if something happened to you, where would you get meds. We go a little bit deeper. We don’t go all the way down to who’s going to help you with toileting, or who’s going to help you get in and out of the bathtub and some of those smaller details. What I find fascinating is that among a lot of my seniors is that they’ve already been caregivers themselves to other family members. Or your 80-year old was taking care of his mom or dad when she had a stroke in the 1980s.
We’re already seeing 2nd generation caregiving. The big thing I see among my seniors is that they don’t want to be a burden on their children. This is a way of thinking ahead and saying, “I don’t want to be a burden on my children, I want to start thinking about this now so that it isn’t a burden.”
I’ve seen sometimes where the family caregiver or the family supporter sits down with the senior and goes through the website. Then they can have a general conversation about what things might look like down the road.
Alex : That’s wonderful. This is terrific work. I have a question about who should use this website. Is this for everybody? For people over a certain age? Is it for people who are at high risk of hospitalization, falls, or Alzheimer’s dementia? What’s your target audience?
Lee : We got a second PCORI grant to do dissemination implementation of planyourlifespan.org. We’ve had hits in about 42 different states, plus three other countries. There’s been over 20,000 hits on the website. We’re seeing people in all age ranges using it. More so people that are 50 plus, 55 plus. Usually what I’m seeing is, is that the 70 and 80 year olds are using it, and talking about it with their children who are in their 50s and 60s. Then the 50s and 60 years olds are using it.
On the fun side, a great pediatrician by the name of Sophia Jan reached out to me, and she’s actually developing this website that parallels ours for people who are aging out of … with autism. So they’re aging out of services, the family’s trying to figure out how to plan ahead. It’s really fascinating how there’s so much planning for health care that we need in multiple ages.
Ken : Lee, this might … I’m going to try to phrase this right, because this might feel a little obscure. As you were talking about this, there’s the plan for your care on the individual level, of these are the circumstances we face in the US, and these are the things that are likely to happen. If there was plan for your care on the societal level, then kind of what I’m driving at is, the way we organize health care. Is health care for seniors actually organized in a way that facilitates planning for the typical needs of the frail elderly? Based on your experience, are there ways we could do better, are there examples from other countries about how we do better in terms of helping people when they reach this phase of life?
Lee : I think that from my standpoint, it’s all about helping to support the caregiver. That’s where I think that most of the movement is. We’ve so many times just been siloed into here’s senior care, here’s adult care, here’s pediatric care. There’s so much of an interchange between the caregivers, which are usually middle-aged adults in the seniors, that I think a lot of improving of senior health care will be also supporting the caregiver, and supporting the social needs.
What I’ve seen in some of the best situations have been where there’s a lot of intergenerational care, meaning that families will not throw the senior to the side, or not automatically put them in a nursing home, but actually keep them in the household, or keep integrating them in their lives. Whether it’s visiting them a couple times a week, or exchanging people who’s going to be taking gramma out to lunch, but just actually embracing seniors. I think that’s something that we need to do as a society more, is to embrace them and keep them involved. Whether it’s taking them to a Cubs game, or taking them out to lunch, or to the Cubs convention. Stuff like that. Or even taking them to Costco.
Alex : More Cubs is better.
Lee : You like my Cubs plug there you guys?
Ken : I’m very impressed.
Lee : I don’t know many seniors who hate the Cubs, and would hate to go to Wrigley Field. I’m just saying! I’m just saying.
I think the other thing, too, that I wanted to push is that on this research that we did in how we built this website, it was very patient centered, so we had so many different community partners. I learned so much from my community partners. I think in research we do so much research oriented or researcher driven, investigator driven work, where the investigator comes up with the idea. On this project, the seniors were really guiding where we go with this, and the family caregivers. So if anyone listens to this podcast, and wants to become a community partner with us, or help us with research, we’d love to hear from you.
Ken : Actually Lee, could you say a few things you learned from your community partners?
Lee : With our community partners we learned so much, because we heard what made them fearful of it, and we heard what a lot of the misconceptions were. We also understood how people wanted to hear things. For instance, people didn’t want to hear this is pre-end-of-life care. They wanted to hear it as, this is just another stage in my life. A lot of people didn’t like talking about aging in place, because people just don’t live in one place. It’s kind of more aging in their own communities.
They also came up with other ideas, because measuring aging in place is another thing that’s tricky. There’s no great scale out there that measures aging in place. We’re coming up with our own promise level measuring aging in place, scale. They’ve helped with the protocols, with recruitment … oh my god, our seniors did so much recruitment for this study that we surpassed our goals within the first few weeks of doing it. They did all the recruitment for us, which was fantastic. We actually got to end early because our recruitment was so good.
Alex : That’s terrific.
Ken : That doesn’t happen often.
Lee : No, we were lucky. A lot of our community partners went out to their friends, and got their own friends involved. These are people that aren’t usually in research, they’re not really tapped in. We had rural partners in Indiana, in Pennsylvania and Texas. We’re partnering now with a great group of people, the First Vitals out in Honolulu. They’re another rural partner that we have.
Eric : A lot of this is patient focused, family focused information that you’re delivering here. Do you have any for our listeners, who are often healthcare providers, one or two things that you’ve learned doing this that they should do in their practice to help patients and family members?
Lee : I usually use the statement, let’s talk about your goals, your advanced care planning, but then let’s also talk to 20 years or 30 years beforehand, or even 10 years, depending on the age of the person. Then I usually say, here’s planyourlifespan.org, go through it, figure it out, look at it with your loved ones. That conversation is less than five minutes, and then the patient can go home with the website, planyourlifespan.org. If anyone is interested in materials, feel free to contact me, because we’ve got a bunch of materials we can send people’s practices, and it’s also available online. Then they can let the seniors and their caregivers go through this themselves.
The other thing that I’ve heard back is that planyourlifespan.org is kind of like a virtual social worker. I’m lucky enough I get to work with a social worker, but not a lot of practices do have social workers in their community based practices. If you don’t know where your area agency on aging is, or how do I get help for my patient on this, it’s just a huge clearing house for resources that’s free to use. It actually is very patient friendly, because it’s written in a very low health literate format, so people can use it at any level of language.
Eric : Lee, anything else you’d like to talk about before we end here?
Lee : Cubs are gonna win next year.
No, thank you so much for having me on. This has been great to have a … to actually be on GeriPal. This is such a hero moment for me, because you guys are the best. I follow you on Twitter, too, so it’s tops on my book. Feel free to visit planyourlifespan.org, and thank you so much for the opportunity to present my work.
Eric : I think you made Ken’s day by picking that song, so how about we end with it.
Ken : Lee, I just wanted to thank you for your work. I just think it’s so important. You’re really kind of hitting on an area that is so much the practice with geriatrics but hasn’t been part of policy planning as much of it should be, and hasn’t been part of our research agenda the way it should be. It’s really just great work.
Lee : Thank you.(singing)
Alex : Yeah, Chicago!
Lee : Yay!



