Much has been written in geriatrics and palliative care about anticipatory grief, about the grief of caregivers, and even the grief clinicians experience following the deaths of their patients. Krista Harrison, in a Piece of My Mind essay in JAMA, writes about something different. She writes about coping, as an academic hospice and palliative care researcher, with personal grief from the deaths of her dad and step-dad within 5 months of each other.
There are many reasons this essay likely touched so many people (it seemed to be all over Twitter). One is that there’s a silence around this experience of death. Krista’s essay opens up a space to talk about it. Another is that the experience of grief is in fact universal, whether it’s the loss of a loved one, the loss of a colleague or mentor to illness or a move, the loss of “a return to normal” following COVID.
Krista wanted to add a couple of things not mentioned in the podcast that she found helpful. First, she treasures videos she has of her loved ones recorded before death. Second, she made fingerprint imprints of her two dads and keeps the fingerprint impressions in a locket around her neck.
We talk with Krista about these and many other things on this week’s podcast. Let’s keep the conversation going.
Links:
- Making Space for Grief in Academia, JAMA
- The Hidden Curriculum of Hospice: Die Fast, Not Slow, Health Affairs
- Live Discharge from Hospice Isn’t Graduating – It’s Getting Expelled, JAGS
- Griefcast podcast
- RadioLab: The Queen of Dying Podcast
- The Dougy Center Grief Out Loud Podcast
- On Being Podcast
- The Five Invitations by Frank Ostaseski
- Resilient Grieving by Lucy Hone
- The Art of Losing (poems)
- When Things Fall Apart by Pema Chodron
Eric: Welcome to the GeriPal podcast. This is Eric Widera.
Alex: This is Alex Smith.
Eric: And Alex, who do we have with us today?
Alex: We are delighted to welcome back to the GeriPal podcast Krista Harrison, who unfortunately we don’t have singing opera with us today as she did, I think, on the first time she was a guest on the GeriPal podcast, who is a researcher, faculty member in the UCSF Division of Geriatrics, and she studies care at home for people living with serious illness, including hospice and other delivery mechanisms. Welcome back to the GeriPal podcast, Krista.
Krista: Thanks for having me.
Eric: Krista, we could have taken this podcast in a lot of different directions. You’ve had a lot of articles come out recently, Health Affairs, JAGS, but this one I think touched a lot of people. I see it popping up on my Twitter feed, like every two minutes I see another person talking about this article. It is a JAMA Piece of My Mind piece called Making Space for Grief in Academia. So that’s our topic today, talking about grief in academics and sharing a little bit about your story and the JAMA paper and a lot more. But before we do, do you have a song request for Alex?
Krista: I do. I would like to request A Long December by the Counting Crows.
Alex: And can you tell us why?
Krista: When I looked up the lyrics, it is actually a story of somebody close to the artist who was in a car accident and was in the hospital for a long time, and in fact, that was a really long December in my family. It was also a song that I didn’t think would make me cry.
Alex: Well, I think I’ll be able to meet that goal, not making you cry. Here we go. (singing).
Krista: Nice.
Alex: Little transposition of words there. Close enough.
Eric: Well, Krista, I’m going to go straight to the JAMA paper. So in this JAMA paper, and you talk about the five months between your son’s 2nd birthday and your 37th, your father and your stepfather died. And I really loved… paragraph through paragraph were very quotable, and it was just an exceptionally beautifully written Piece of My Mind. I’m just going to give our reviewers one taste. She said, “Losing parents is so terribly ordinary. Much like becoming a parent, these acute losses come with learning a new way of being, a new language. The world is split into before and after.” Do you want to, just for our audience, just describe a little bit about kind of the losses that you experienced at this time?
Krista: Sure. I mean, it’s a surprising five months to say the least. In some ways, the story starts a few months prior when my stepfather, who was dying of a neurodegenerative disease, we think it was multiple system atrophy where he had lots of functional impairment but no minimal cognitive impairment, he was hospitalized from breathing problems. And so I had flown down, and actually must’ve been exactly three years ago this past week or this weekend that I was helping with his hospital discharge. And I was asking about, “Well, where’s your palliative care service? Where’s your home-based care service?” because clearly I’ve spent too much time at UCSF. And they said, “Yeah, we only have it for oncology here,” and “We can send you home with home health, but you can’t get services for a few days.”
Krista: And so there were weeks of waking up to emojis from my mother, indicating that my stepfather was still alive. My father was postponing a visit out to see us because we thought I’d be flying back across the country anytime because my stepfather would have died. And then one day I was sitting in my office in Laurel Heights and I got a call from my brother. And actually Alex, I think, was my first or second call to just… because Alex was also a cyclist, to find out what the heck was I hearing. So I eternally appreciate that, Alex.
Krista: And it was… My dad was hit. My dad and three friends were hit while riding bikes. And my dad was a huge cyclist, thousands and thousands of miles a year. And a car who, also relevant to our geriatrics audience, was an 80-year-old driver who was visually impaired driving into the sun at 8:00 in the morning in Florida, who presumably hadn’t seen them. And my dad was the only one who died to catastrophic neck injuries, and amazingly the people he was riding with who also were in the trauma ICU ended up riding again. I follow them on Strava.
Krista: And so there was sort of a five-day period where we debated when to go out, debated what to do, got to appreciate the actual palliative care skills of the neurosurgeon who talked to us, got to request a couple of family meetings, got to request that palliative care get involved even though the trauma ICU was not a big fan. And then… so it was a case of needing to make… it was a very clear decision to make, but making a decision to do the palliative extubation, and then…
Krista: …yeah, it’s funny. I don’t talk about this that much. I’ve written about it, but I don’t actually talk about it that much. And then, skipping ahead, it was… My stepfather three or four months later got kicked out of hospice for extended prognosis. That was not well-telegraphed in advance, and so it was a traumatic transition, and then there was another emergency flight back across the country when probably a UTI was really severe and finally made a decision, all right, we’re not going to treat this one with antibiotics. And he was able to communicate enough with a board because the neurodegenerative disease meant he couldn’t talk anymore, but he was able to use a communication board that we had created to say he was okay with not treating it. So that’s when we re-enrolled with hospice, and I was not there for that. I actually wasn’t present for either death, but for Larry’s, I wasn’t in the state.
Eric: You said the losses just kept on coming too afterwards as well.
Krista: Yeah, it was unfortunate that one of my primary mentors and collaborators ended up leaving for another institution. And that was an amazing opportunity for that person, and I was thrilled in our… We had a big team and our team moved on to new opportunities and that was great for them, but for me, it just became these additional destabilizations of everyday life. And then my uncle died of sepsis, a high school friend died of cancer, a cousin died of cancer, the latter two both my age with young kids around the age of my son, my next door neighbor… so I got to help with, in the beginning of the pandemic, bringing in the hospice bed, all these opportunities for re-triggering. Yeah.
Eric: Mm-hmm (affirmative). And, you know, Alex and I always feel differently about authors reading from their stories, but I’m going to throw Alex a bone. Do you have the paper in front of you, Krista?
Krista: I do.
Eric: Would you just mind reading the paragraph that starts with academic rewards?
Krista: Academia rewards those who can make hardship invisible, who can be productive amid and despite crisis. Colleagues told me to take the time I needed, yet what I needed seemed unknowable. It was my second year on faculty in a soft money environment. I needed grants to have a job the following year. I remember sitting on my mother’s couch in Florida, toggling between writing my dad’s obituary, helping with my stepfather’s breathing treatments, and editing a grant due in two weeks, my son asleep on my lap. Meeting deadlines felt easier than requesting extensions, than explaining. Academic parenting, sandwich generationing, left no room for processing.
Eric: For timing, was this also all taking place during the pandemic, or was this pre…
Krista: No, this was… This was 2018, that particular paragraph. Yeah, it’s probably a bad sign when you can say 2020 was the best of the last three years.
Alex: Krista, let me just say thank you so much for coming on this podcast and talking about this challenging issue. Takes a lot of courage and strength to be able to talk about something so personal and so shatteringly devastating at that time in your life with our audience, so thank you for that. I wanted to ask what you… Looking back now, you said, “What I needed seemed unknowable.” I wonder if you could say a little bit about what you did get, what advice or what thoughts or what listening ears, what were helpful and what maybe wasn’t, anonymized, of course. Really.
Krista: Yeah, so it’s funny. I was thinking about, I was no stranger to death. You know, I had lost all four grandparents within the prior 10 years, an uncle. The death of my grandmother was the reason I went into hospice and took a job in hospice, and then ultimately came into hospice research and to UCSF. So in some ways, it’s strange to me at how different this was, but I think it was both the sudden loss and the unexpected loss and the intertwining of the losses with my professional life that just made it a whole different ballpark, and absent people having sort of their own list, their own roadmap that they could give to me. I probably had one of the best-case scenarios with you all being experts in geriatrics and palliative care, and so many of our colleagues both locally and across the US having been through their own losses. And so I did get a lot of one-on-one advice and support.
Krista: So for example, you told me, what are you doing for self-care? And that’s the line in the piece where I said, wait, what are the options? Because I was in a very deep hole of just trying to get through the day-to-day and it didn’t occur to me I didn’t know where to start. And others really insisted that I take time off, and I think somebody must have given me some ideas of what the heck to do with that time, because I didn’t know and I really had to learn how to step outside the day-to-day and find ways to face the feelings, feel the feelings.
Krista: Somebody told me, schedule time on the calendar to just feel the feelings as hard as you can and cry, and then go back to the workday, which seemed so ridiculous at the time, but actually surprisingly very helpful. Having a menu of opportunities of things I could do, to choose from based on the mood, learning to ignore the shoulds, like I should do this, I should feel better if I do this, and just sort of operate on instinct of, well, this made me feel better, or this feels like the right approach today, and maybe it’ll feel different tomorrow.
Krista: But in addition, finding ways to hire help, finding ways to reduce the number of things I was doing. I think I cleared my schedule for the first month or two and just wrote one paper, which was partly just to practice some version of normalcy, but it was also… That was about all I could handle, even though I couldn’t articulate that at the time. And I hired help to collect data that I was supposed to collect, but it was all supposed to be interviews with bereaved caregivers of people who had died of dementia. It was not a good idea.
Alex: Right.
Eric: Let me ask you this too. You write in this that academia must shift the norms and expectations around loss and bereavement. Are there things that you think should have happened? I know this is touchy, like you are… a conflict of interest statement is that we’re all UCSF employees, but I think this article is resonating because I think everybody feels something about this article that resonates with them. It makes sense. So when you think about the institutions that we work with, what do you think we need to change?
Krista: There were times where there just felt like there was such judgment if you said you were reducing… if I said I was reducing my workload or changing the status quo, and I don’t think it was meant, but it’s how I interpreted whatever was being said. And I think… I wish there was some way to be able to really reduce what is expected of us, the volume in particular, so that we have more flexibility, because, frankly, self-care takes an immense amount of time, especially when you’re working out of a huge well of need. And I had the luck of being able to have flexibility. There’s a massive ebb and flow to a researcher’s life, where there are times where you work intensely and you’re really productive and times where you’re not, and I wish that everybody had this, and I know it’s not.
Krista: While I was backpacking, which was happening when the article came out, I was thinking about how our leaders necessarily can’t have all the experiences of the people that they are supporting, and that it’s often people who are in leadership, who are maybe farther away from those particularly hard life experiences, whether losing a parent or caregiving or caregiving for a child or caregiving for somebody who is seriously ill in their family, and I was thinking, I wish there was some way to have advisory boards that aren’t made up of just similar level experts, but actually people from different stages of their careers, different parts of their life experiences, who can say, “Here are the hardships I’m encountering,” and then there could be a brainstorming of, great, let’s think of some innovative ways to make space for this.
Krista: It feels like there would need to be a way to… I don’t know, like average out our productivity goals for over two years or something, right? Like you need to hit these benchmarks. We don’t care about the hours. Something like that, but I don’t know how to do it, but that’s why bringing together a group of innovative people from different walks of life to figure it out would be kind of cool.
Eric: Yeah. I think another thing that resonated with me in this article is that you also talk about all the different losses. It wasn’t just of your dad, but so many, like even your colleague went to another institution. I feel like over the last year and a half with COVID, I feel like, for me in particular, I had a tremendous amount of energy when the pandemic first hit, and there are surges in New York and Alex and I volunteered virtually in New York, and like so much energy. We’re going to get through this. Let’s bring down that curve, then the pandemic kept on going, and then in December, like, hey, we got vaccines now. We’re going to get everybody vaccinated. Come July, it was like a reprieve. Hey, things are opening up, this is ending, and we had two glorious weeks in July where COVID was ending and we were going to all meet in person and we all envisioned a life that looked probably a lot like our lives before COVID.
Eric: And then summer hit, and Southeast got hammered. We’re coming to a realization that COVID is probably endemic. We’re going to live like this before… and much like grief, you don’t go back to the old. You don’t go back to who you were before. You’re in this new normal state, and I feel like you got… Grief is adaptive. It’s healthy, and we got to acknowledge it and work through it in some ways to come to that new normal state. And I think for me, again, we’re probably all reading this and interpreting it differently, like different pieces are resonating. That’s the part for me that resonated hard, that I’m actually grieving right now what I thought my future would be, and recognizing now it’s very different.
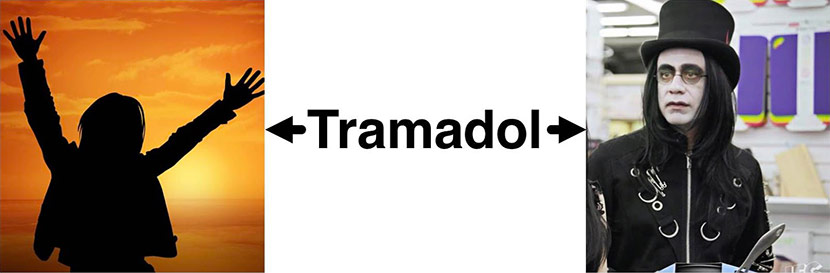
Krista: Yeah. I said this in a Twitter thread that I sent out today, but I’ve been very into the grief podcasts because they’ve helped give me the roadmap that I wasn’t getting anywhere else. There was a lot of talk at the start of the pandemic of, oh, this is familiar. This feels like grieving. And so that makes a lot of sense to me. I’ve always, since being in this new world, I’ve liked the concept of the ancillary losses, the secondary losses. So it’s, for me, in the very proximate sense, it’s not just I’ve lost my dad, but I’ve also lost the person I could call when I was in Ace Hardware looking for that thing. How am I supposed to use this? There’s those things that we can’t do in the same ways that we used to.
Krista: I also liked the concept in grief that it’s not that we are healed. It’s not that we move on. It’s that we grow around this loss, that you… The loss becomes smaller because you become bigger as you reinvent yourself. So it’s not really a recovery. It’s a reinvention, and I think that that, for me, also has been holding true about the pandemic, of what do I want my life to look like in the next six months or in the next two years, and how does that compare? But there’s a lot of uncertainty because we don’t know what’s coming down the pipe and what it’s going to feel like.
Eric: I guess one question to you, Krista, is that, for a lot of healthcare providers, they’re dealing with people who are incredibly sick, like for myself coming from a very privileged location. And sometimes it’s hard to acknowledge our own grief and losses when we see so much suffering out there. In some ways, we’re trying to compare suffering. As a doctor, we’re always comparing and it’s hard not to, but my suffering does not even come close to what they’re dealing with. So in a way, we’re kind of minimizing our own loss and our grief despite actually potentially it being very… an important loss to us. Does that ring true at all, or any thoughts on that from your own experiences?
Krista: Yeah, I think it’s so tempting to feel like I shouldn’t be grieving this because whatever, right? Fill in the blank. And the truth is, though, your feelings don’t really care about that intellectual point of view, and that if we don’t make space for those feelings, it’s… I like the phrase grief waits to be heard. It waits till you take the time and the space to honor whatever it is you’re feeling, regardless of how it compares to the rest of the world. I’ve also found solace over time in talking to people with proximate experiences to mine for that reason, so there’s less of that comparing.
Krista: It’s just… So you asked earlier about what other supports I wished existed that were easy to access. I was surprised that there weren’t a slew of grief support groups, university affiliated or supported somehow. And so I think I’ve ended up with a variety of peer support groups, and in those, there’s been a lot of talking about, the comparisons aren’t helpful here compared to just honoring the way you’re feeling. I also feel like each of these losses gives me a little more empathy for what other people are going through, which is, as you said, the fact that I’m still in academia on the other side of these losses represents the amount of privilege of my situation and the supports that were available to me.
Krista: Being in that position is also what inspired me to try to make things better insofar as I can for the people who are in more precarious positions or who are dealing with more, because if the stuff that I dealt with, which was a lot in a small amount of time, but let me tell you, I’m hearing stories of plenty worse, plenty more concentrated or more sudden. So we need those people contributing to a more compassionate society.
Eric: Yeah. It always reminds me too, and I think of worse suffering, less suffering, it reminds me of a story. BJ Miller once shared about, he was giving a talk… and we’ve had BJ on our podcast. He was talking about suffering and people share different stories of suffering, and there were terrible things going on, tremendous amount of suffering that people were sharing. And at the end, somebody walked up to BJ and said, “You know what? I just… I feel really bad. Just, I haven’t suffered. I haven’t… I heard these terrible stories and I haven’t suffered.” And BJ turns to them and said, “I can see you’re suffering right now. The way that you are feeling it, like you’re suffering.” And again, BJ describes this much better than I did.
Eric: And it just again reminds me, is that I think it’s human nature in a way to try to in a way grade of levels of suffering, and in the end, grief is so individualized. Like you said, it’s about your feelings, this usually adaptive, healthy response to an important loss, and you can’t grade what’s important. Somebody else can’t grade what’s important. And I think it’s just reading your article too, and the other things that we know, like anniversaries just bring up these grief responses. I loved in your article… I was like, you also talked about you doing this type of academic work that involves a lot of death and dying also brings up this grief response. Is that right? Or potentially maybe doing a podcast on it.
Krista: Yeah. It gave me a new respect for my palliative care and hospice colleagues, let me tell you, how you make space for your personal losses amid your professional losses that, I mean, are necessitated in an environment…
Eric: You mean that small little ball that I crunch things deep inside and don’t open it up until it blows up somewhere else-
Krista: That’s very healthy, Eric. [laughter]
Alex: That’s the one.
Eric: … that little space that I keep for all the stuff?
Alex: You know, Krista, one of the things that strikes me as being innovative, novel, and maybe one of the reasons this has resonated so widely with people, is that in geriatrics, palliative care, hospice, we write, think about research patients with serious illness and their anticipatory grief, the grief of caregivers after the death of their loved one. We write and think about how clinicians may become burnt out, as Eric was alluding to, from caring for people with serious illness and the deaths of those people, and that little knot of grief that accumulates over time is packed away in the closet until it falls on your head.
Alex: And what you’ve done is something different, which is to write about your personal experiences of grief and academics, and I think that’s a space that hasn’t been opened up before, and that’s maybe one of the reasons that your article resonated so widely. And that also, for you, seems to have been a coping mechanism, writing about the grief experience. And I know this is one of about three papers that I’m aware of that sort of touches on this, this paper and your Health Affairs paper, which is… These are great titles. The Health Affairs paper is The Hidden Curriculum of Hospice: Die Fast, Not Slow. And then your paper with Lauren Hunt in JAGS, Live discharge from hospice for people living with dementia isn’t graduating – It’s getting expelled. I wonder if you could talk with our listeners about the process of academic writing about your grief experience.
Krista: Yeah. Thanks for that question. It was an interesting… It wasn’t a conscious decision, and people have asked, “Was it a cathartic thing or was it hard?” No, it was just the thing. The effort was about getting it right and about… It’s probably some amount of wanting to be a mechanism of transformation or to use this awfulness to catalyze change. The first two paragraphs of the JAMA piece came out pretty intact the night my stepfather died, and then what ended up being most of the end of the Health Affairs piece came out a few weeks later. And then it was just a matter of trying to figure out, what am I really trying to say, and what am I going to do with this? What is the point of this?
Krista: I think what helped me persist in tinkering and submitting was watching other friends go through sudden losses and their similar bewilderment with, “Wait, I’m supposed to go back to meetings now? People are asking me to do things? How do I… They’re asking me if I’m okay now? This is crazy.” And remembering that those early days of grief and wanting it to be, again, wanting it to be different for other people. In the case of my stepfather, because it was so entwined with my professional research and career trajectory, it was really knowing, and it probably helps that my predilection is for qualitative research, but knowing the importance of combining stories with numbers in order to advocate for change, actually, both the qualitative background and the policy background, right? That’s how you get policy change too, is good stories and good data.
Krista: And then with the JAMA piece in particular, my father was a poet, not a great one and not a well-published one, but nonetheless a persistent and lifelong poet. I similarly wrote probably fairly mediocre poetry up through college. So this was the closest it had gotten back to that. So it felt like a very familiar way of processing and seeing the world in a different way and transforming it through words.
Alex: Mm-hmm (affirmative). Yeah, I’m a persistent guitar player. I wonder if there’s a new Twitter-length phrase here. What is the… The existing phrase is something like, women grieve alone, men grieve in others’ arms, and academics grieve by writing about it. But it is true that there are so many folks I’ve met who are practicing in hospice and palliative medicine and geriatrics, who are doing research on those issues, have had… They’re fueled by their personal experiences. It gives it this authenticity, and as Ken Covinsky likes to say, we’ve drunk the Kool-Aid. I laud you for the way that you’ve processed or sublimated or whatever the psychological word is, that experience and those emotions and the deep work that you’ve done of reflection and sharing it with others so that they can benefit from you. So I just want to say thank you to that.
Krista: Thank you. It’s making me think that maybe some journal editor could put out a call for origin stories in hospice, geriatrics, and palliative care, or the personal motivations behind. It would be really cool to hear those origin stories, because I feel like when I came from health services research and policy research to the geriatrics, hospice, and palliative care side of things, that all of a sudden I was saying, wait, we’re allowed to tell stories about how personal experiences motivated our research? Really?
Alex: Right, right.
Eric: I was bitten by a radioactive spider. That’s my origin story. [laughter]
Alex: Gave you palliative care super powers, podcasting powers. [laughter]
Krista: You got a sibling that makes super suits.
Alex: I wanted to ask if there… I remember you were reading books early on, and I know we didn’t talk about in advance, so you may not remember titles or anything off the cuff, but I wonder if, for our listeners, are there any you recall that were particularly helpful that you’d recommend?
Krista: Yeah. I really liked Resilient Grieving, who I think was by Lena Horne. In fact, there’s probably a copy that is in your office at the VA. I bought a bunch of copies. They’ve been distributed around to… bought more copies for myself. It probably is that it resonated with my… It was also a researcher who experienced a sudden loss, but it’s a very type A sort of like, okay, I’m going to figure out, how do I recover and reintegrate as most efficiently as possible? Very, very true to my particular form of grieving, so yeah.
Alex: Yeah, I can see that.
Eric: I just got to do these tasks. I got my little check boxes and then I will be moving into acceptance very quickly from denial, bargaining, anger. Let’s just get through those four stages real quick so I get to accept it. [laughter]
Krista: Those stages have not resonated for me, I got to say. I’ve… They just… It is so iterative, in and out, backwards and forwards, upwards and down. I also discovered… people sent me things, so there was a book of poetry called The Art of Losing, which was a compilation of poems about loss that I really liked. Somebody sent me Pema Chodron’s When Things Fall Apart, which I had never read before but ended up being a nice match. Frank — and I can’t pronounce his last name, Frank O’s The Five Invitations. It’s pretty good, actually.
Alex: Ostaseski? He was in hospice?
Krista: Yeah, who turns out is a neighbor of mine on the houseboats in Sausalito.
Alex: I didn’t know you were there.
Eric: So I’m guessing the people who are listening to us on our podcast like also listening to podcasts. I’m going to throw one out there. I really love… So Radiolab, one of my favorite podcasts, they had an episode on the queen of dying. I think this is mandatory podcast listening for anybody who does palliative care or hospice care about Elizabeth Kubler-Ross, the five stages, and also talks about how you don’t walk through five stages. But it was absolutely a fascinating podcast. What other podcasts? You mentioned one before. Was it the grief podcast?
Krista: The Griefcast out of Britain.
Eric: The Griefcast.
Krista: Yep, I highly recommend it. It’s comedians talking with other comedians and people who are grieving, and I have just found that to be a great one. The Dougy Center has a…
Eric: Dougy Center?
Krista: Mm-hmm (affirmative).
Eric: Like Doogie Howser?
Krista: Yep.
Eric: All right. Dougy Center.
Krista: They support grieving and loss for young adults, which turns out to be 40 and younger, which I liked that definition. They have the Grief Out Loud podcast that is also really great. And again, I sort of go with the things that are resonating with me, so I’ve discovered as I’ve looked for them a whole lot more options. I also found that On Being is another podcast that periodically has topics that really resonate and help with my grief understanding and journey.
Eric: Can I ask you one more favor? Can you read this second to the last paragraph?
Krista: Yep. When the coronavirus pandemic began, I relearned, expanded, and shared this menu of coping practices and resources with colleagues and friends navigating their own losses. I’ve heard these resources have been further passed along to other grievers and pandemic survivors. I became the one cautiously sharing my own experience of how I learned to live and laugh amid loss and uncertainty, to accept the duality of, and oscillations between, being okay and not. Vulnerability itself can be a gift, normalizing loss and reintegration.
Eric: Yeah, that was just, for me that was just a stunning paragraph to read and it brought up a lot of thoughts. I think it shows both how good of a writer you are and also the expertise you’ve built around this topic as well. You have a role too now within our own division around wellness. Do you think that there are things, not big institutions, but even smaller divisions or sections, that we should be doing to help in these situations?
Krista: One, stop asking how people are and start asking a more answerable question. I’ve been leaning towards, “How’s your concentration today?” or “How big are the emotions today?” It’s more of a silly answer in some ways, but I have been surprised by how much people feel alone in what are common experiences, whether it’s feeling like they can’t do something as well as they want to, or the losses, or the struggles with pandemic parenting, and how much… not venting, but normalizing those experiences and sharing ways that each of us are coping with them and bouncing ideas off of each other of how to make it through this really complicated, hard time that is constantly shifting has been incredibly powerful.
Krista: And I’ve been trying to help others set up groups for themselves, because of course the things that resonate for me are not things that necessarily resonate for you. And so people have to be figuring out their own groups of people who are going to help them persist but also step their game up a little, and not just in a professional sense but in their whole selves, trying to… because if you’re trying to juggle grief and parenting and the world falling apart around you and show up and pretend none of that’s happening at work, yeah, you might be able to do that for a bit, but it’s not going to be for long.
Eric: Yeah, and I just love how intertwined it’s all… As a new parent or a parent of a child in school, part of your grief, maybe I just want this kid to have a normal life, like to be able to school, or for me to actually just think, every day I’m not worried if he’s going to be quarantined or she’s going to be quarantined for two weeks. All of those are losses and they may be important losses. Like you said, we’re all dealing with something.
Eric: With that, I just want to really, really thank you for publishing this and having the courage to do that. That’s the other part I loved about the second last paragraph, that vulnerability itself can be a gift, normalizing loss and reintegration. I think part of what you did is normalize that we’re all dealing with this, so thank you. Before we leave, though-
Krista: Thank you for making space for this conversation.
Eric: … Alex, a little bit more of Long December?
Alex: A little bit more. (singing – with with repeated ending). Sorry, I’m just messing with Eric. He’s like, when is this song going to end? [laughing]
Eric: I let Krista read twice. [laughing]
Eric: Alex and I were having a discussion before this podcast about whether or not people like listening to authors read from their book. I was firmly in the camp of no, Alex firmly in the camp of yes. So…
Eric: I do have to say, I thought it worked really well today-
Alex: It did.
Eric: … so there you go, Alex. Krista, very big thank you-
Alex: Thank you, Krista.
Eric: … and for reading so lovely from your JAMA article, but really also for being vulnerable and talking about this on a podcast and the JAMA paper and everything else, because it is very much a gift, so thank you.
Krista: I appreciate that. Thank you.
Eric: Thank you, Archstone Foundation, for your continued support of this GeriPal podcast. And all of our listeners, we hope you are all doing the best that you can in these troubling times, and I hope you give yourself some space today too. Bye, everybody.