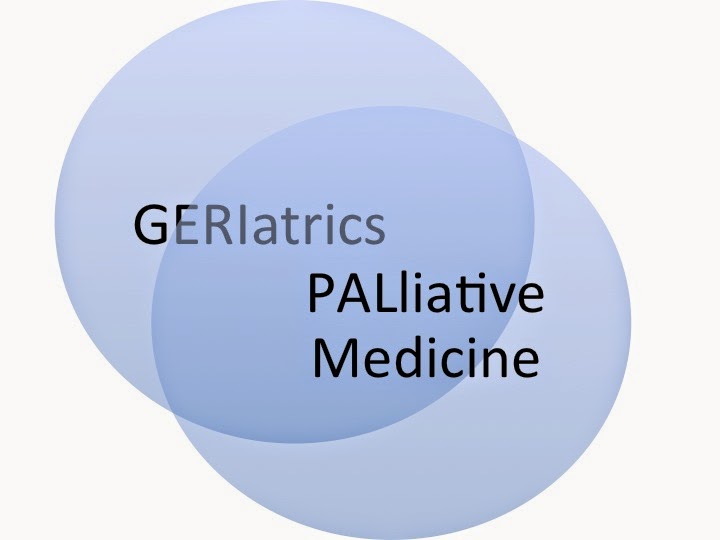
Over the past decade, the disciplines of Geriatrics and
Palliative Medicine have become intellectual cousins.
Within Palliative Medicine, the recognition that Palliative
Medicine is not just about end of life care has been a paradigm shift. There is now recognition that core skills of
Palliative Medicine, including symptom management, communication, and caregiver
support are needed throughout the course of serious illness. While these needs of seriously ill patients transcend
age, it is a demographic fact that older persons will be the bulk of persons
with these chronic palliative care needs. So, the population that has long been of interest to Geriatrics is now
of great interest to Palliative Medicine.
Within Geriatrics, we have become consumed with the
recognition that most frail older persons have multiple illnesses. We realize that treating each illness
separately, rather than treating the whole patient leads to considerable
harm. Geriatricians strongly advocate for a focus on
whole person health outcomes such quality of life and functional status rather
than traditional disease metrics. Geriatricians
have been increasingly concerned that traditional treatments focused on each
individual diagnosis leads to dangerous levels of overtreatment that can harm
patients.
On the other hand, care that is grounded in an understanding
of the patient’s goals, focused on quality of life, functional, and supportive
needs of the patient and caregiver is of great benefit. Kind of sounds like we are getting pretty
close to palliative care, doesn’t it? So
a basic competency of Geriatrics is the ability to attend to the palliative
needs of frail patients throughout the full course of serious
illness
So, given this overlap between the two fields, shouldn’t the
next step for each field be to aggressively define and defend its turf?
Two wonderful perspectives, by Jim Pacala and Diane Meier in
the Journal of the American Geriatrics Society, eloquently argue that the
answer to this question is an emphatic NO! These thoughtful perspectives are great reading for those in both
fields.
Pacala and Meier implore us to put a laser focus on the
needs of seriously ill patients, rather than worry about who has what turf. Both
fields focus on the most vulnerable patients, the 5% of patients who consume
50% of health costs. Yet for all that
money, our health system is utterly failing these vulnerable patients,
delivering disjointed, dysfunctional care that does not meet their needs and
goals, and often causes harm rather than benefit. We should of course embrace what is unique
about each discipline and value the specialized
skills each discipline may bring to the table. But, Pacala and Meier tell us that we have so much more to gain by
collaborating and working together than worrying about turf.
Perhaps the most important feature that unites those in
Geriatrics and Palliative Medicine is the passionate belief that we need to
change how health care is delivered to seriously ill patients. With needs so great, we do not need to worry
about turf. There is more than enough
work to go around. By working together,
we can offer hope to seriously ill patients and their caregivers who feel that
their voices are not being heard.
by: Ken Covinsky @geri_doc