“He’d feel okay about not replacing the pacemaker’s battery when it ran down, he said. But turning it off, he said, would be “too active.” Later he would tell me that it would have been “like putting a pillow over your father’s head.”
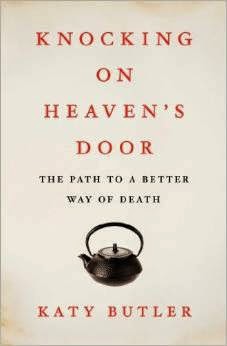
These are the words of Katy Butler in her book “Knocking on Heaven’s Door – The Path to a Better Way of Death” in which she writes about her families ordeal in trying to have her father’s pacemaker. It is also something that I’m hearing more about, in particular health care professionals refusing to deactivate a pacemaker due to concerns that doing so would be akin to euthenasia.
Separating Euthanasia and Deactivation
Why is pacemaker deactivation neither physician-assisted suicide nor euthanasia? I think one of the easiest ways to look at it is by asking what is the intent of a particular intervention and what are the means that will be used to meet that intent. For both physician-assisted suicide and euthanasia the outcome that is intended is the relief of suffering through death. However, the primary intent in pacemaker deactivation is to respect the patient and surrogates request to discontinue the unwanted treatment. The intent is not to terminate the patient’s life, although death may be an anticipated outcome in those who are at least significantly pacer dependent. Additionally and very importantly, death is not the means to meeting the intent of deactivation.
If it isn’t euthanasia, is it ethical to deactivate a pacemaker?
It is very clear that many physicians have moral distress over deactivation of a pacemaker. Studies have shown that many physicians view cardiovascular implantable electronic devices as distinct from other life-sustaining therapies. Furthermore there is a view that pacemakers are different from AICDs or other medical interventions commonly withdrawn as the end of life, as a pacemaker replaces a natural cardiac physiology, it is automatic, it is implanted, and its action is not felt by the patient.
The problem with this viewpoint is that there is very little to support it either ethically or legally. Patients have the right to refuse or withdraw treatments, even if the treatment prolongs life and immediate death would follow a decision not to use it. This applies to ventilatory support, dialysis, AICDs, or pacemakers. Nor does it matter if a patient has an underlying rhythm that is incompatible with life. If this were true, ventilator withdrawal or discontinuation of dialysis would also be limited to those who are healthy enough to survive extubation or dialysis discontinuation.
Furthermore, if it is believed that the patient could have initially refused placement of a pacemaker, there is little justification that she (or her surrogate) can now no longer discontinue it. Continuation of her life was equally dependent previously on the placement of the pacemaker as it is now on continuation of the pacemaker function.
What to do when a health care provider refuses deactivation?
Send them to the experts. I would print them out the recent expert consensus statement from Heart Rhythm Society written in written in collaboration with representatives the American College of Cardiology (ACC), the American Geriatrics Society (AGS), the American Academy of Hospice and Palliative Medicine (AAHPM); the American Heart Association (AHA), the European Heart Rhythm Association (EHRA), and the Hospice and Palliative Nurses Association (HPNA). Key points from this very in-depth statement include:
- “A patient with decision-making capacity has the legal right to refuse or
request the withdrawal of any medical treatment or intervention, regardless of
whether s/he is terminally ill, and regardless of whether the treatment prolongs
life and its withdrawal results in death.” - “When a patient lacks capacity, his/her legally-defined surrogate decision-
maker has the same right to refuse or request the withdrawal of treatment as the
patient would have if the patient had decision-making capacity.” - “Legally, carrying out a request to withdraw life-sustaining treatment is
neither physician-assisted suicide nor euthanasia.” - “The right to refuse or request the withdrawal of a treatment is a personal
right of the patient and does not depend on the characteristics of the
particular treatment involved (i.e., CIEDs). Therefore, no treatment, including
CIED therapies, has unique ethical or legal status.”
by: Eric Widera (@ewidera)
NOTE: Comment on any of the pacemaker posts this week or talk about it on twitter and you’ll be entered into a drawing to win one of the paperback versions of Katy Butler’s book “Knocking on Heaven’s Door: The Path to a Better Way of Death.”