When have advance directives ever been shown to do anything? They were a complete failure in SUPPORT. Study after study demonstrates that few people fill them out, rarely are they used, and that health care proxies don’t have a great idea of what their loved one want anyway. As Angela Fagerlin and Carl Schnieder famously opined: “Enough: Failure of the Living Will.”
And yet, over the last few years a series of studies have breathed new life into advance directives (see here and here). A new studypublished today in JAMA adds another piece to the puzzle. The challenge is that it’s a somewhat puzzling piece.
A terrific group of researchers from the University of Michigan used a nationally representative survey of older adults followed through death. They examined variation in medical expenditures for persons with advance directives that state treatment should be limited in certain situations, to those without advance directives or advance directives stating no limitations in care. They found:
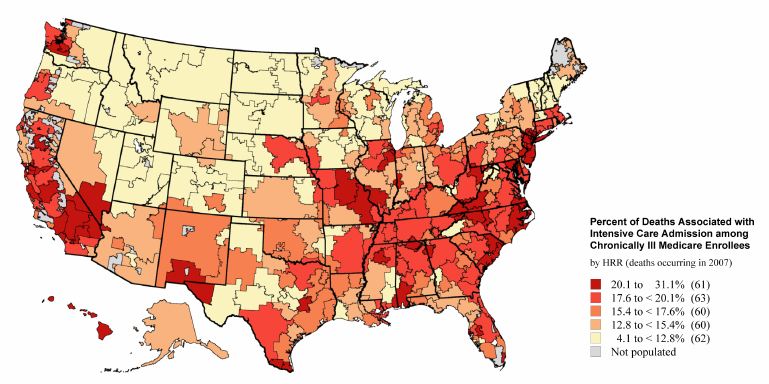
- Advance directives specifying limitations in end-of-life care were associated with lower costs in regions where end-of-life care spending was highest, but not in middle or low spending regions.
- No difference in use of life-sustaining treatments (intubation, mechanical ventilation, treacheostomy, gastrostomy tube placement, hemodialysis, tpn, CPR) by advance directive status, across all spending regions.
- People with advance directives specifying limitations were more likely to use hospice and die outside of the hospital in high spending regions.
So what to make of this? The authors argue that advance directives seem
to have the most impact when they specify a direction of care that is
“counter-culture” – limiting life-sustaining treatments in an area
where costly end-of-life care is the norm (sorry to pick on you New
York and Los Angeles!).
We have more help in interpreting these findings in the accompanying editorial by Doug White and Bob Arnold. They argue that while the initiation of life-sustaining treatments does not entirely explain differences in the impact of advance care planning on costs in high spending regions (as no difference was found), perhaps the duration of use of life support explains differences in cost:
Advance directives were originally designed to allow patients to determine in advance what treatment they would receive in the event of their incapacity. Instead, it may be that treatment-limiting advance directives work not by making the decisions but by giving surrogates and physicians psychological permission to cease life support at some point…This distinction is important because it may signal the need to refocus advance care planning efforts to help surrogates and clinicians make good decisions rather than simply enact patients’ prior decisions.
This is a very interesting observation, and bears repeating in light of Rebecca Sudore and Terri Fried’s work: advance directives help surrogates make in-the-moment decisions. Deciding not to initiate life-support is hard, and I know many family members (including my own) who could not say no to initiating these treatments in the crunch of the moment…even if the advance directive specified avoiding those treatments. Because, really, who knows? Maybe the directive didn’t apply to this exact scenario? Maybe there’s a chance? But after the initial storm, advance directives offer some guidance, allowing loved one’s permission to agree to a time-limited trial. And then, when the trajectory is more certain, to let go.
by: Alex Smith