Cannabis use by older adults has increased substantially over the last decade, a trend that has paralleled the legalization of its use for medical and recreational purposes. In that same time, there has been a decreased perceived risk associated with cannabis use in older adults as noted in a recent study published in JAGS.
On today’s podcast we talk with Drs. Bree Johnston and Ben Han about what the health care providers role is in cannabinoid prescribing and advising when caring for older adults.
We try to cover a lot in this podcast, including some of these topics:
- Epidemiology of cannabis used by older adults (including aspects of the JAGS study)
- The basic pharmacology and dosing of cannabinoids
- The latest evidence for the efficacy of cannabis
- Specific risks and side effects that providers should be aware about, and how we should monitor patients using cannabinoid products
- Drug interactions we should be aware about
Eric: Welcome to the GeriPal Podcast, this is Eric Widera.
Alex: This is Alex Smith.
Eric: And Alex, who do we have with us today?
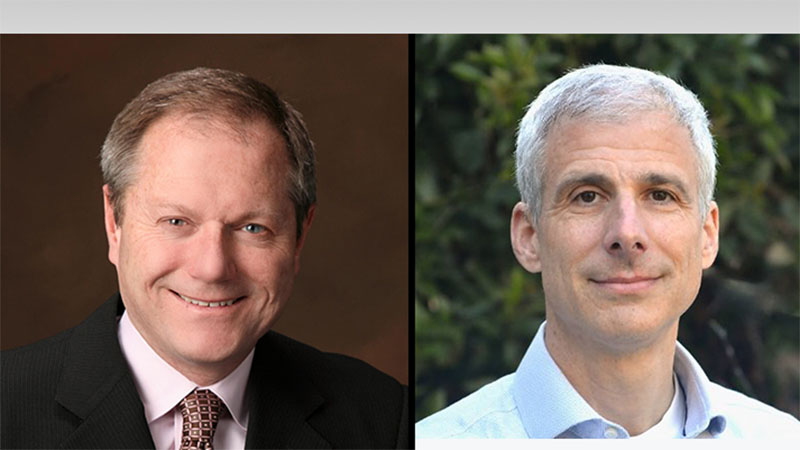
Alex: It warms my heart to welcome Bree Johnston to the GeriPal Podcast. Bree is the director of palliative care at Skagit Regional Health in Washington State and a professor of medicine at the University of Arizona, and was a long, long time faculty at the UCSF Division of Geriatrics. Welcome to the GeriPal podcast, Bree.
Bree: It’s so fun to be here.
Eric: When I was a medical student way back when, Bree was my attending, and then when I was a fellow, Bree was my attending, and now as we talk about this topic, Bree is going to continue to be my attending. [laughter]
Alex: That’s right. We’re also delighted to welcome Ben Han, who has been on the podcast before. He’s an assistant professor at UCSD, he’s a geriatrician, and specializes in addiction medicine, and we’ve had him on before about this topic, and delighted to welcome you back, Ben.
Ben: Great to be here again, thank you.
Eric: So we’re going to be talking about cannabis. Uses in the medical sphere, and also in older adults, but before we talk about this, do you got a song request? I think, Bree, you got a song request for Alex.
Bree: There were so many good possibilities … the Grateful Dead, Tom Petty, Lil Wayne, Snoop Dogg. But I think we’ve got to go with the Dylan, and Rainy Day Women.
Alex: You got to go with Rainy Day Women? Okay, here’s a snippet.
Alex: (singing)
Eric: I am not even going to ask why you picked that song, Bree. [laughter] All right, before we start, I want to make sure whatever term I’m using is the current correct term. Medical marijuana, cannabis, what should I be calling this-
Alex: The GeriPal Doobie Podcast? [laugher]
Bree: I would vote for medical cannabis.
Eric: Medical cannabis. Ben? Medical cannabis?
Ben: Yeah, I also try to only use cannabis mainly because marijuana, the term marijuana, has very racist roots, and I associate it a lot with kind of the racist prohibition, criminalization of cannabis, and so especially in addiction medicine, we try to use less stigmatizing terms. And so cannabis, I think, is more … well, specifically accurate, I think it is more accurate and less stigmatizing. So I tend to use cannabis.
Bree: Well put, Ben.
Eric: And when we’re using the word cannabis, we’re talking about all of the many different compounds that are in the cannabis plant? What is the definition for cannabis? Right? There’s cannabinoids, there’s THC, all of that is … is cannabis just referring to the plant?
Bree: I think there’s probably a loose definition, but when I talk about cannabinoids, I think about both the medical compounds as well as the whole plant, and many of the compounds in the plant. Although the plants have other compounds as well, some turpenoids and flavinoids. But I think it’s just kind of a general term.
Alex: It’s kind of like opioids, and opiates, and they’re synthetic-
Eric: Don’t even get started with that, Alex.
Alex: You got to use the right term, Eric. [laughter]
Eric: You got to, we’re going to get hate mail if you use the wrong opioid term. [laughter]
Alex: Wait, I want to hear more … Ben, you mentioned that there’s a sort of racist legacy to the term marijuana. I was unaware of this, I don’t know if either of you can say a little bit more about that?
Ben: So, I’m not a historical expert on this, but from what I’ve read, cannabis started … I think it goes back to, when cannabis was coming from Mexico, a couple hundred years ago, and the term marijuana was I guess more derogatory towards Mexicans who were coming to the United States? I think that’s where the term really kind of started to arise from. I don’t know, Bree, if you know.
Bree: I think that’s absolutely right, and I can’t tell you the year, but that term was specifically introduced to try to stigmatize cannabinoids. So I would agree, that unless you’re having fun somewhere, I would stick with the term cannabinoids.
Alex: All right, thank you.
Eric: All right, so we will stick to this podcast using the word cannabis. Not weed, not marijuana, not pot, not chronic. Cannabis.
Eric: So, Bree, you just gave an amazing ACP talk on this subject. Part of the reason that came up for the talk about it here on the GeriPal Podcast. How did you get interested in this as a subject? Why present this at ACP?
Bree: How did I get interested in this? … I know, I know. So you all don’t know me as a cannabis expert at all, and the reason why I took this on is cannabis was legalized in Washington state in 2012. And when I came up here to work from UCSF, I found so many of my patients were using cannabinoids, and I think it was in 2016, I had a couple of weeks when every single patient I saw was taking cannabinoids, and they’d all ask me my opinion. And I got sick of saying, “I don’t know.” So, I had a summer where I wasn’t doing that much other stuff, and I just took courses and read everything I could, and I decided I am going to learn about this. And I found it’s really hard to get a good handle on the research and the medical, the true medical indications, and I think there are a lot of reasons for that, that we could get into later.
Bree: And just so you know, I’m not a stoner. I don’t do well on cannabis myself, I kind of get paranoid. So, that wasn’t the rationale.
Eric: Well, Ben, how about you? How did you … you’re coming from this from a research perspective around older adults, and we’ve had you on the podcast before, how did you get interested in this as a subject?
Ben: So yes, I’m, as a geriatrician and addiction medicine physician, this is certainly an area that I’m interested in. I’m really focused on … mainly my research focuses on improving the health of older adults with substance abuse disorders, or people with chronic diseases. But, cannabis is really … when you’re looking at different substances among older adults, cannabis seems to be, aside from alcohol and tobacco, one of the ones with a really rising prevalence. And so, this is an area that as a geriatrician I wanted to explore more.
Eric: And as a geriatrician, and as a researcher, who’s published a lot on this including a JAMA IM piece last year, and a JAGS piece which we’ll be talking about this year, plus multiple other pieces. How common is the use of cannabis in older adults?
Ben: So we’ve been, as part of my research we’ve been tracking, monitoring the prevalence of cannabis among older adults in the United States, and going back about 15 years, so 2006, we looked at, using national surveys we looked at the prevalence of past 12 month use of cannabis among people 65 years of age and older, again from a nationally represented survey. And the prevalence in 2006 was less than 0.4% had used cannabis in the past 12 months.
Alex: That’s really low, yeah, almost zero.
Ben: Almost zero. And so for the paper we published last year in JAMA Internal Medicine, we looked at the data up to 2018 and the prevalence had increased to 4.2%. And the more recent data from 2019 shows that among adults aged 65 and older, the prevalence is now over 5%. So, while it’s still relatively low, so in comparison adults age 18-25, the prevalence is more like 33, 35%? In terms of relative increase over this time, really we’re seeing the largest increase among older adults.
Alex: Yeah, and do you think … are you able to break it down by states and seeing that in states that have legalized cannabis for medical or recreational purposes that it’s gone up more dramatically among older adults?
Ben: So we haven’t looked at that directly, and in our studies another limitation is we can’t tell if someone is using it for recreational purposes or medical purposes. But other studies have shown, it’s a little bit hard to kind of track those based on states. Other people have tried, but.
Eric: You’ve done some other studies with other authors looking at use of cannabis for treating from a medical perspective, right? For treating symptoms? Is that right, Ben?
Ben: Not to my … not really.
Eric: I thought there was another JAGS article from last year looking at the treatment of common symptoms in older adults and the use of cannabis.
Ben: Oh, right, right. Oh yeah, sorry. I totally forgot about that.[laughter]
Eric: Sorry, that was a little bit too leading of a question, I should’ve actually said what I wanted to say. [laughter]
Ben: So yeah, so that paper, my co-authors here at UCSD gave a survey to older adults from the geriatric medicine clinic her, trying to just get a sense of why people are using it, how they’re using it, and so it seemed like the most common reason for using it was for chronic pain, or sleep, or anxiety. Those are the most common reasons, at least from this sample.
Eric: All right, Bree, now I’m going to turn to you. Does it work for those things? What’s the evidence base for cannabis for the treatment of all of these things? If you talk to some of the proponents, it seems like the miracle drug that fixes everything.
Bree: Right, right.
Eric: Is it?
Bree: I think the evidence is mixed. So the evidence is really good for neuropathic pain. The evidence is more mixed for chronic pain, if you actually look at the randomized trials. But let’s just back up and talk about the limitations of cannabis trials. Many of these trials use synthetic marinol, some of them use nabixomols, which is a combination THC/CBD thing.
Eric: Just real quick, marinol is just synthetic THC, right?
Bree: It’s a synthetic THC, right.
Eric: Okay.
Bree: So, when you’re looking at the study, and in the United States until very recently there was mainly one strain that was being used that was manufactured at the University of Mississippi. So, if you look at what is happening in the legal states, there are all these different cultivars. If you look at what’s happening in research, we’re looking at a very narrow window, many of the trials are very small and underpowered. So, we really are only looking at the tip of the iceberg when we look at evidence. And Ben, would you agree with that more or less?
Ben: Right, yeah, I agree. And I think as, I do primary care and also I do research, and I think what I expect when I practice medicine, I try to do as much evidence-based medicine as possible, and it’s really hard because of the limitations and the available studies. The studies use different types of cannabis, they use different ratios, they get different outcomes, the followup period aren’t that long, and if you look at randomized control trials, there are not too many people in them that we expect from other therapeutics. And so, yeah, there’s a lot we don’t know, and so it’s hard to recommend things to patients to balance kind of the benefits and the risks.
Bree: And so we’re in this really screwy situation where we have tons of anecdotal data. So everybody has an opinion, but we have very little high quality data. So it makes it really hard to tease out what the truth is. But with that as background-
Eric: Real quick, Bree, so just so I have a little … as you talk about that, the evidence. So there is, it’s the type of drug, right? So is it mainly THC, is it CBD? What’s the ratio of the different CBDs, right?
Bree: Right.
Eric: And then the route, too, right? So lots of different routs you could potentially give this in through?
Bree: So there are lots of different routes. You can do sublingual, you can smoke it, you can orally ingest it which has a different metabolism. You can do it topically, you can use suppositories. So, there are all this different routes. And then the other thing is that the medical, like marinol, that’s THC. Whole plant is a much more complex plant, and depending on the cultivar you’re looking at, you’re going to have different turpenoids, cannabinoids, and flavinoids in there that may make markedly different symptoms. For example, for a long time people talked about the Indica versus the Sativa variety. And Indica is the sedating variety, and that’s largely due to some of the other compounds in the plant, not just the THC and the CBD as opposed to Sativa, which is much more activating. So even if you were doing a trial with those two, you might come out with different results. So, I think there are huge caveats when we talk about what is the evidence.
Alex: I liked in your PowerPoint slides, Indica, also known as In-da-couch, the sedating variety, and then Sativa, what was that one?
Bree: Saturday night.
Alex: Saturday night? [laughing]
Bree: Yeah. Yeah. So, yeah, that’s the only way I could remember them.
Bree: So the evidence is very strong for nausea and vomiting, neuropathic pain, spasticity, and multiple sclerosis. For CBD, there’s very good evidence about seizures and in childhood syndromes. There’s also some evidence about Tourette’s syndrome. Now, the evidence on chronic pain is much more mixed. If you separate out the neuropathic pain trials and the chronic pain trials, the chronic pain trials tend to have much weaker evidence and confidence intervals that often cross one. But, that may not be the whole story. Because when you talk to patients, they say, “My pain’s just as bad, but I don’t care as much.” So people talk about something called the entourage effect with whole plant, whereas if you’re making pain a little better, anxiety a little better, sleep a little better, you may be improving quality of life overall, even though you may not show a statistically significant improvement in pain.
Bree: Now, that’s a theory, but if you look at some of the epidemiologic evidence, and there’s some really good studies that were published in Health Affairs in 2016 and 2017, if you look at states that passed cannabis laws, prescriptions for pain went way down and opioid deaths went down.
Alex: Wow.
Bree: So that’s really suggestive that even though the RCTs haven’t been showing a benefit, that there’s something going on there.
Eric: Mm-hmm (affirmative). That is fascinating. What about for other conditions like mental health issues like anxiety? Especially with 2020, a lot of anxiety out there. Do we have any evidence around treatment?
Bree: So, this is one where there’s just tons of anecdotal evidence that people get benefit related to their anxiety, particularly with CBD. But the randomized evidence just isn’t there. Ben, what do you see?
Ben: Yeah, I agree. I agree.
Alex: And, well speaking of which, Ben, do you have any early evidence about what happened to epidemiology of cannabis use during the COVID epidemic?
Ben: That, I don’t have yet.
Alex: Not yet, yeah. Because I would suspect that it went up.
Ben: Right.
Alex: Yup, as other drugs have went up, alcohol in particular.
Ben: Right, right.
Bree: Yeah, those of us who are paranoid on cannabis if we’re alone all the time, it doesn’t really matter as much.
Eric: Right.
Alex: Bree-
Bree: That was a joke, Alex. [laughter]
Eric: All right, Bree. Nausea and vomiting. So this is the one where were have marinol out there, and I got to say, I’ve used it, not for myself but for my patients. Never really got a lot of positive feedback that it works really well. But, the anecdotal data that I get around people using the cannabis products themselves? Great anecdotal feedback that I’m getting from individuals when they use it. Thoughts on cannabis for nausea and vomiting?
Bree: So we have nabalone, which is a really, really expensive drug that it has proved for chemotherapy, improved nausea and vomiting. We have marinol, which is also approved, and it’s approved for AIDS-related wasting.
Eric: And what’s the difference between those two?
Bree: Nabalone and marinol?
Eric: Yeah.
Bree: Basically the price. No, they’re different synthetic THCs, but nabalone is really expensive, and I think-
Bree: It’s really expensive andit’s made a lot of money.
Eric: Yeah.
Bree: I think, for many of our patients, I talk about symptom complexes that are often helpful, and often for our patients who are going through chemotherapy I find cannabinoids can be really helpful, just because of anxiety, pain, nausea, and vomiting. So I agree with you, Eric, that even patients that don’t find a benefit with marinol many times do find benefit with whole plant therapy.
Alex: So what do you recommend that they purchase? Because if it’s whole plant, that’s something we don’t prescribe, am I right? That’s something they would get from a medical dispensary.
Bree: This is tricky. I mean, it’s trick because there’s so many unknowns, so any recommendation I make is with a lot of caveats, that we don’t know, and depending on what state you’re in, it’s not always clear that what’s on the product label is the actual dose. It really varies from state to state how tightly regulated it is. So you have to do this with a lot of caveats.
Bree: I think if you are in a state where it’s legal, it’s helpful to find a dispensary where you find somebody who’s knowledgeable and who you kind of trust. And then, if you have a dispensary like that, I will often ask them to find a product. I often think that oral sprays, or sublingual formulations are nice because you don’t have the smoking, and the pharmacology’s a little more straightforward than ingested. Often, with a combination THC/CBD product, and I often will tell people, just give a trial dose at 2.5 milligrams a night and see how you feel on it.
Bree: People vary so widely in their responses to cannabinoid products. Some people love the way they feel, other people feel panicky, some people feel paranoid. So it depends on the dose, the person, the indication and the product, so it’s incredibly complicated.
Eric: And do we know anything about how age plays a role in that, as people get older?
Alex: Do they have stronger reactions one way or the other?
Bree: So, I want to talk about a mouse study that’s really interesting. There’s a really interesting mouse study, and I don’t know if anyone has looked at this in humans, but they looked at learning on young mice and old mice on cannabinoids, and they found that the young mice had impairments in their learning, and they found that the old mice had enhancements in learning. So, we know that the endocannabinoid receptors decline with aging. So I think it’s plausible to think that probably there’s a difference across the lifespan. But I don’t think we really know what it is. There is some published literature about older people, and clearly balance gets impaired and some cognition gets impaired, so I think older people do have to use it with caution.
Bree: Ben, what would you say about that?
Ben: So I think, I worry about any substance or medication with psychoactive properties in older adults. I think, in my experience older adults tend to be more sensitive to alcohol for instance. I don’t know specifically about cannabis, but I would worry … because, especially the THC component has psychoactive properties, I worry about it a little bit more for my older patients. And again, as you said, I really start low and go slow, so I really start the THC, I tell them to try to start at two and a half, and then kind of go up, gradually up from there.
Eric: Mm-hmm (affirmative).
Alex: Bree, you were saying by way of the introduction that you had one week where every patient of yours, I presume this was on palliative care?
Bree: Yeah.
Alex: Yeah, on palliative care. And Ben talked about how nationally, rates among older adults are somewhere about 5% in national surveys. And among people with serious illness, it’s got to be higher. I mean, I don’t know that anyone’s done the study, but I’ve had so many patients ask about it, patients who are either were already taking cannabinoids with, or are interested in starting them in the setting of serious illness. I’ve had several patients who’ve said, “Hey, this is my opportunity to try it, I’ve wanted to try it my whole life, and now I feel like I have permission to do it because I have a serious illness. That usually doesn’t work out so well. I’ve had several experience where patients, “Oh, this is nothing like I was anticipating. I had never used it before, and this is definitely not for me.” But I just feel like the prevalence among people with serious illness must be … I don’t know, 50%? Something really high.
Bree: And I think so too. And another thing I’m seeing a lot of, I would be really interested in what you’re all seeing, is a lot of people trying it for the neurobehavioral symptoms of dementia, particularly trying CBD. So there’s a lot of that out there.
Eric: Yeah, I feel like use of CBD is … I mean, you can just go to a grocery store where I live and buy some CBD and talk to the person behind the counter, they tell you which one to buy out of the 20 different combos that they have up on the wall.
Alex: And to talk to the person behind the counter is key, especially in these dispensaries. Bree, you had a picture in your PowerPoint slide like, who do your patients go to for advice about this. Is it the doctor? No. It’s the person at the dispensary, right? That’s who’s giving … that’s who’s the authority for these patients. And there are a lot of reasons for that, and one is as doctors, we’re used to giving evidence based recommendations, but people behind the dispensary, they’re giving recommendations, I don’t know what they’re saying.
Bree: And I think that’s one of the impossible situations we’re in. We’ve been totally handicapped by the fact that cannabinoids are still scheduled as a schedule one drug, which means there’s no legitimate use for them, and because research is so hampered, just the anecdotal data is far ahead of what we can offer.
Eric: Can I ask about that? Because I feel like I can get CBD anywhere. I’m not sure they have it at CostCo, but I mean it’s-
Bree: They do.
Eric: … what size CBD must be, right? Just gigantic bottles of different types of CBD at CostCo. [laughter] Is it the THC, what is the scheduled component? How come I can buy it at CostCo, CBD, but if it has THC it’s-
Alex: Maybe it’s because you live in California, Eric.
Bree: Yeah, and I don’t know all the ins and outs of this, but it’s the THC component, and one of the things that’s happening is cannabis is in the hemp family. So, hemp has to be produced with I think less than .5% THC or something like that, some very low quantity. So, there are many states where you can get hemp, but not medical cannabis. But what people have started doing is realizing that hemp has delta-8 THC, which is similar to delta-9 THC and has some psychoactive properties. So, people are, in states where it’s illegal, are using that. That’s really unregulated. From one batch to the next you could have a 20-fold difference in what you’re getting. So that complicates it too.
Eric: So if I’m wearing my hemp shirt right now, I can just smoke it if I’m in a state that doesn’t allow it.
Bree: Yeah.
Eric: Real quick, what are the … we talked about benefits, or some of the issues, are there any harms of using medical cannabis?
Bree: Yes. So, I think particularly in younger people. So the epidemiologic association between cannabis use and schizophrenia is really strong. And there could be confounding, but if you look at it, there’s a dose response. So young people who use cannabis tend to have twice the rate of schizophrenia. They tend to have onset two years earlier, and if you look at the highest use people, the risk is even higher than that. There may be some associated with learning disabilities. I think that’s much more likely to be associated with compounding. There’s something called the cannabis hyperemesis syndrome, where people who chronically use can have a situation where they get nausea all the time relieved with hot showers, that’s pathic mnemonic. And then there are other, more mild associations and I’m sure Ben has much more to say on this.
Ben: Right, so with anything, there’s risks. Any therapeutic, any medication has some kind of inherent risk. So again, I worry a lot about the psychoactive properties among older adults who may be more sensitive to it, so I hear a lot about, “I tried cannabis, it made me very dizzy, I fell down,” I worry about that. I also worry about the co-use of cannabis with other psychoactive medications, so using it with alcohol, or using it with benzodiazepines could cause issues for older adults. There have been some suggestion that it might cause, affect blood pressure, can cause orthostatic hypotension, may increase heart rate. I haven’t seen those things clinically, but these are some things that are suggested in the literature. And also, a main one is also driving.
Alex: Yeah, driving.
Ben: So driving while using cannabis, your risk for a car accident’s much higher. So that’s also another risk as well.
Alex: Is there some safe level or is there no safe level, and what do you tell your patients when you prescribe cannabis.
Ben: I worry. I mean I recommend, just like alcohol, I recommend if you’re going to drink, don’t drive. I recommend the same thing with cannabis. It’s very variable, as Bree has mentioned. How it affects one person, it may affect someone else very differently, and also how you use it. So I’ve had patients who tried a cookie, because when you ingest it, the peak plasma level might not come until a couple hours later, and so you may not feel effects right away. So I’ve had patients … they don’t feel anything after 15 minutes, and then they eat the whole cookie, and then three hours later they end up in the emergency room, or they had a very bad experience with it. And so especially ingesting it, because it also can last longer and it’s such a variable, you kind of don’t know how you’re going to respond to it. Yeah, so it’s really hard to tell. So in general, I just tell patients if you’re going to try cannabis, especially with THC contents, to avoid driving at that time.
Bree: I would totally agree with that. And Colorado did designate a safe level, but I think there was an interesting study that was done, actually. They looked at accidents on 4/20, the date, and they compared it to the day before and the day after, and they found that traffic accidents went way up, but particularly among the youngest, most inexperienced drivers. So-
Eric: Is that the day that it was legalized, or something?
Bree: No, that’s-
Alex: Oh, that’s a day. That’s a-
Bree: That’s cannabis day, or green … I don’t know.
Eric: Yeah. I don’t … right, it’s that day.
Bree: It’s that day.
Eric: I don’t remember what that day is called either. Oh, that’s interesting.
Bree: … I know of at least one instance where there was an older woman who was taking 400 milligrams of THC daily, and was admitted with a psychotic episode. And I don’t think we’re hearing about that much of those kinds of things, but I think they happen.
Alex: How about lung disease? Mark Plancher published on this a few years ago as I recall, in JAMA. I can’t remember, I remember the headlines were like, it’s not as bad as we thought?
Bree: Yeah.
Eric: And certainly not as bad as smoking?
Bree: Yeah. If you look at it, there is an increase in phlegm production and cough, but so far nobody’s demonstrated an increase of COPD or lung cancer, and the same as Ben said, there were some old studies suggesting that particularly probably when people take really high dose of THC that there’s increased risk of heart attack and maybe cardiac events in the hour following. If you look at that over broad population, it’s hard to see anything.
Eric: And Ben, you just published an article in Journal of American Geriatric Society, JAGS, Decreasing Perceived Risk of Regular Cannabis Use Amongst Older Adults, 2015-2019. Do you want to tell us a little bit about what you found?
Ben: Sure. So this was using, again, a national survey that specifically asked everyone how much do people risk harming themselves physically or in other ways when they smoke marijuana once or twice a week. And so it’s really getting at the perceived risk associated with regular cannabis use. And the reason we decided to look at this question was because I was seeing in clinic, a lot of patients were hesitant to continue a statin, or metformin because they had a perceived risk associated with it. But then with cannabis, they have … at least for the patients I see, they have very low perceived risk of cannabis. They think, “Oh, it’s everywhere, people are using it, there’s no harm to it.” Which is, as we just discussed, that’s not the case. And so that’s why we decided to look at this question, and in previous studies show that older adults had the highest perceived risk of cannabis.
Ben: And so we wanted to see if that’s changed over a five year period, up to 2019, and really the perceived risk nationally among older adults has decreased about 20%. And really, specifically among certain groups of older people, people who binge drink, people who use tobacco, you have a sharper decrease of the perceived risk of cannabis, regular cannabis use. But also among people with certain chronic diseases, people with two or more chronic diseases, people with chronic lung disease, which … it’s not clear there are potential harms, respiratory harms, but I do worry about my patients who have COPD, if they smoke cannabis it might trigger, might irritate the airways.
Ben: So, I guess the bottom line for our study was that everything has risks. It’s important that patients know that, know that there are potential risk with cannabis, and it’s important to kind of weigh the benefits and the risks when using it. And so it’s, nothing is 100% risk-free.
Bree: I think there’s another risk that I worry about. I don’t know if this has been true of the three of you, but I’ve had many, maybe not many, but I would say up to 10 patients who have declined getting treatments for cancer because they’ve heard about Rick Simpson oil, or these high potency cannabinoids that they think are going to cure their cancer. So I think some of the false hype is actually a harm, it actually puts people at risk.
Eric: Rick Simpson oil?
Bree: Rick Simpson oil.
Ben: Another risk I should mention, as an addiction medicine physician, is cannabis use disorder is a real thing. People do have cannabis use disorder, and have problematic use with cannabis, and so, and we’re seeing an increase in that. And so that’s also another potential risk of using cannabis.
Alex: Now Ben, in your study, I don’t know if … I should know this, having read your study, but are we able to tease out whether this is a generational effect, in that as we, the population ages and people who were born and went through the ’60s are moving into old age, we’ll have greater, less perceived risk with cannabis? Or is this attitudes changing among the same people over time?
Ben: Right, so I think it probably is a little bit of both, probably more so we’re seeing a generational shift, especially with the baby boomer generation. Definitely has different perceptions towards substance use compared to earlier generations [inaudible 00:39:08]. I think we’re seeing both of those things.
Alex: Right, and then could this be … what is the phrase? Canary in the coal mine, that it’s likely that attitudes change first and then use of cannabinoids will follow?
Ben: Right, right. Yeah, that’s one of the reasons we wanted to look at this, because if someone’s risk perception can influence certain health behaviors such as substance use, so [inaudible 00:39:37].
Eric: All right, one of my last questions. We just did a podcast about polypharmacy and de-prescribing. What’s the risk for people taking a lot of different medications? Are there a lot of drug-drug interactions we have to worry about?
Bree: The biggest drug-drug interactions are actually with the CBD component, more with the THC, although I would echo what Ben says, that if you’re adding cannabis to any other psychoactive medicine, especially in older people, you are probably going to increase the risk of cognitive outcomes, dizziness, falls.
Eric: And with CBD are there particular medicines you worry about, Bree?
Bree: Yeah, so there’s a lot of use of CBD for seizure disorders, and actually CBD really interacts with a lot of the anti-seizure medicines. So, I would really encourage anybody who’s using them for that indication to be really, really careful. So that’s really my biggest concerns. But any of the cytochrome P450 drugs, there’s a potential for an interaction.
Eric: Mm-hmm (affirmative).
Bree: Depending on the minor pathway.
Eric: Mm-hmm (affirmative).
Alex: So, I just want to help our listeners who are overwhelmingly clinicians caring for older adults or people with serious illness. Let’s say you have a patient coming to you, an older adult, who has cancer and is interested in using cannabinoid to control their nausea and vomiting and neuropathic pain. Recommended starting dose? Aspirationally it’d be great if the clinician went out and formed a relationship with a local dispensary, but failing that, they want to just prescribe something, and they’re in a state where it’s legal, medical use of cannabis is legal. What should they prescribe as a starting point? You said 2.5 of … what do they write on the paper?
Bree: Well, so you don’t really write the prescription … well, depending on if you have a dispensary. But what I would say is 2.5 milligrams, either something sublingual, or what I really like the best is the spray that’s like nabixomols, which is a one to one THC/CBD. But, I would say that with all of the caveats. Will they hear any of the caveats? I don’t know.
Eric: Yeah.
Eric: And how often do they use it?
Bree: I would start at 2.5 milligrams at night, see what the response is. If they tolerate it, try 2.5 twice a day, and then go up to 2.5 three times a day. If you look at the study of cannabinoids with older people, the risk of dizziness and cognitive problems really go up above 10 milligrams. So I would try to stay below 10 milligrams a day if they can get some symptom relief there. If people can tolerate it, sure. They could push it up a little, but the risk is going to go up particularly in older people.
Eric: Mm-hmm (affirmative).
Eric: And Ben, from your standpoint, any kind of key take-homes that you have around cannabis use in older adults?
Ben: So I would say that while cannabis may benefit especially older adults who have chronic diseases, chronic symptoms, there are risks to it. Nothing is risk-free, and so that’s something to be very cautious about, especially for older adults. And very important not to try, not mixing cannabis with other substances like alcohol or benzodiazepines as well.
Alex: Mm-hmm (affirmative). And do you have any pointers, clinician, as a patient, who is using cannabis to the point where it’s an addiction and they want to get off of it? Any thoughts or pointers about helping them with that sort of situation?
Ben: Right, so there isn’t … so there isn’t … so the evidence for people with cannabis use disorder is mostly behavioral interventions, psychotherapy’s really kind of the mainstay at this point. There isn’t a medication like-
Alex: There’s no Nicorette gum or Antabuse equivalent.
Ben: Right, right. So, yeah, so that’s kind of the mainstay. It is an area that’s still developing.
Alex: Mm-hmm (affirmative).
Bree: And Ben, I’ve heard it said, and I don’t know if this is true that if you can try to just wean them off the THC component just to the CBD, that might be a reasonable harm reduction way to begin.
Ben: Right, right, absolutely.
Eric: And Bree, my last question for you. You’re seeing this patient. Let’s say you are recommending somebody with neuropathic pain that they start this one to one combination THC/CBD. You’re giving them good guidance and counseling. Do you put this under their med list? How do you actually let other people know that you’re … do you even put it in your medications? Where does it go in the EMR?
Bree: I think ideally this goes under the herbs and supplements part of the medical record, which not all medical records have. I think if you put it under the substance use part, you really stigmatize people who are using it for a legitimate medical reason. So I like to be honest in my notes. So I would put it under herbs and supplements. If your electronic medical record doesn’t have a section for that, try to add one.
Eric: Mm-hmm (affirmative). Well, I want to thank you both.
Eric: Thank you.
Eric: We can end with a little bit more Dylan before we say goodbye.
Alex: Little bit more Bob Dylan, appropriately chosen.
Alex: (singing)
Eric: Ben and Bree, big thank you for joining us on this GeriPal Podcast.
Bree: Thank you, this was lots of fun.
Eric: Thank you ArchStone Foundation for continued support, and thank you to all of our listeners. Please subscribe to our podcast on YouTube if you have a moment. Try to increase our numbers there. Thanks everybody, have a great night.
Alex: Thank you.