Eight of the 10 largest outbreaks in the US have been in correctional facilities. Physical distancing is impossible in prisons and jails – they’re not built for it. Walkways 3 feet wide. Bunk beds where you can feel your neighbor’s breath. To compound the issue, prisoners are afraid that if they admit they’re sick they will be “put in the hole” (solitary confinement). So they don’t admit when they’re sick.Many people think of prisons as disconnected from society. Like a cruise ship. “It’s happening between those walls, behind the barbed wire, not out here.” But for every two people in a correctional facility there’s about 1 person who works in the correctional facility and lives in the community. The workers are bringing whatever they’ve been exposed to in prison out into the community, and bringing whatever they’ve been exposed to in the community into the prisons. This is a national problem, not a prison or a jail problem.
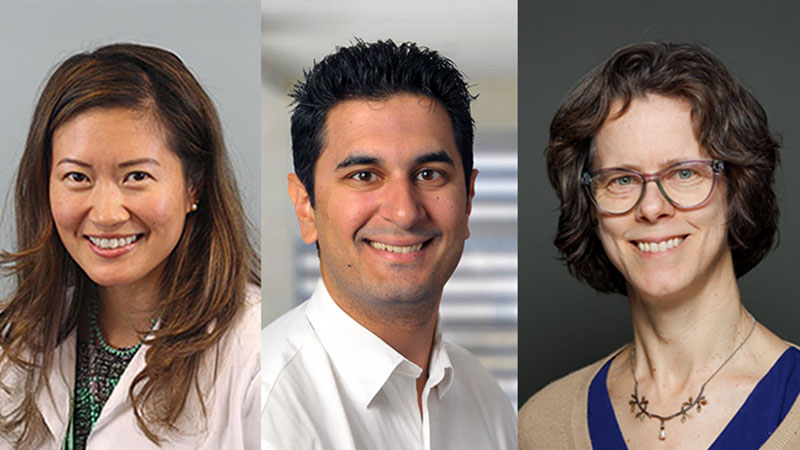
We learned about these critical issues in our podcast with Brie Williams, Professor of Medicine in the UCSF Division of Geriatrics and Director of Amend, a program to change correctional culture; Adnan Khan, Executive Director of Re:store Justice, a justice advocacy organization; and Eric Maserati-E Abercrombie, a singer/songwriter and filmmaker through First Watch, a media project of currently and formerly incarcerated filmmakers. Adnan and Eric Maserati-E are former inmates of San Quentin prison.
What can we do about this? The major response should be decarceration. Reduce the crowding in our overcrowded correctional facilities. If prisoners have less than a year left, let them out. If they have a long sentence and are low risk to society, and a place to go, let them go home with an ankle bracelet and return later to complete their sentence.
Brie reminds us that people in prison can make an advance care plan, they can sign an advance directive, they have the right to engage in goals of care decisions, and a right to elect someone to be their health care proxy. And everybody, including prisoners, has a right to say goodbye to their loved one, though it may be by phone or video.
We learn about these and other critical steps we need to take as a society and as hospice and palliative care clinicians.
Eric Maserati-E does the music for this one. He needs to be discovered! If you know someone in the music industry, make them listen to him. Check out and subscribe to Eric’s YouTube channel. Also, listen to this terrific podcast, Ear Hustle, produced from inside San Quentin, the latest episode featuring Eric’s music.
-@AlexSmithMD
Eric: Welcome to the GeriPal Podcast. This is Eric Widera.
Alex: This is Alex Smith.
Eric: And, Alex, we have an amazing selection of guests with us today.
Alex: We’re fortunate to be joined by Brie Williams, who is professor of medicine at UCSF in the division of geriatrics, and a colleague of Eric and myself, who is also Director of Amend, which is a program to change the correctional culture. Welcome to the GeriPal Podcast, Brie.
Brie: Thanks. It’s good to be here.
Alex: And we have joining us Adnan Khan, who is the Executive Director of Restore Justice, which is a justice advocacy organization. And you can find him on Twitter at @akhan1437. Welcome to the GeriPal Podcast, Adnan.
Adnan: Thank you. Thank you so much for having me.
Alex: And we also have joining us, Eric Maserati-E Abercrombie, who is a singer song writer and filmmaker, and will be doing our music today, which is awesome. And he’s recently doing some film work through First Watch Media, which is an organization of currently and formerly incarcerated filmmakers. You can find him on Twitter at @maserati__e. Welcome to the GeriPal Podcast, Eric.
Eric M.: Hey. Hey, thanks for having me. Thanks for having me.
Eric: We’re going to be talking about COVID19 in prisons. I’m really excited to hear about this topic and talk about it. Alex and I were originally going to go into two different prisons a couple of months ago, but then the pandemic hit and took that off, so I’m really excited to talk about this. And I think this is the first podcast where Alex isn’t doing the singing.
Alex: To clarify, Guy Mico sang once.
Eric: All right. And I guess I sing in the background a couple of times.
Alex: That’s right. Yeah.
Eric: Eric, do you want to tell us a little bit about the song you’re going to sing to us?
Eric M.: Absolutely. This song is called One Day. I wrote it while I still was incarcerated, and it’s really just geared towards hope, resilience, if we will, and illuminating a lot of blind spots in the world when it comes to systemic oppression and various things, if we will. Right? But I think the main take away from it, again, is just hope of that change, that one day things will definitely be different if we continue to strive and push for that difference.
Eric: Great. Let’s hear a little.
Eric M.: Absolutely.
Eric M.: (singing)
Eric: Oh, that was so good. That was great.
Brie: Absolutely.
Alex: I loved it. You need to be discovered big time.
Eric: Where can we find your music?
Alex: You heard it first on the GeriPal Podcast.
Eric: Eric, where can we find your music?
Eric M.: As of now the only place you can find my music is on YouTube, as of right now. I just recently started a YouTube channel. I got a lot of push from that video right there from my boy, Adnan. And, yeah, thank you for that type of motivation. But, yeah, I just recently started a YouTube channel where you’ll be able to find me and my guitar doing all my music acoustically.
Eric: Wonderful.
Eric M.: I do have a project coming out soon, not a certified date just yet waiting on a few more things, but I will be dropping the EP on all major platforms called Going Through Hell To Get To Heaven.
Eric: And we’ll have a link to your YouTube channel on our show notes at GeriPal, and I really want to appreciate it. Alex, I know you were thinking about trying to do one of the songs but I’m so happy Eric joined us. That was-
Alex: The original is always better than my cover, but never more so than in this case. That was terrific. I’m so glad you could join us.
Eric M.: Thanks for having me, man. Definitely. Thanks for having me.
Alex: And we’ll have more at the end.
Eric M.: Absolutely.
Eric: Let’s dive into the topic about COVID19 and prisons in the United States. This doesn’t get a lot of light shined onto it. And I think probably most of us, including myself, I don’t hear much about what’s going on in prisons. You hear about all these other things, so can you just… I’m going to have you, maybe Brie, to start off with. What is going on right now with COVID19 in prisons?
Brie: It’s deeply, deeply troubling. Honestly, not unexpected because these are incredibly densely populated places where people eat, sleep, recreate together and often frequently unsanitary, often overcrowded places. There are a lot of people who are older or who have serious or chronic illnesses, who are very prone getting very sick if they get infected with COVID-19. But right now eight of the 10 of the nation’s biggest outbreaks are in prisons or jails. The communities, the rural communities, that have the biggest outbreaks are either home to meat packing plants.
Brie: Sometimes they’re getting a lot of press, but more frequently are home to prisons or jails, one of the 5,000 prisons or jails around the nation. And so this is a massive problem that is… it’s shocking that it is not front and center. We’re not going to be able to bend the curve of the epidemic until we bend the curve of the epidemic inside prisons and jails. And it is absolutely horrifying and terrifying for the staff, the health care staff, and the residents who live in these places.
Alex: And maybe we could turn from that to talk about what it’s like to be in one of these places, because I want to bring Adnan Khan into this conversation here. You were incarcerated in San Quentin, as well as Eric Maserati-E. I wonder if you could, maybe starting with Adnan, tell us what it’s like in a prison. What puts people at particular risk? What’s a day in the life like, and what are you hearing from people who you might know who are still inside?
Adnan: Yeah. Just to build a little bit more context about me, at the age of 18 I was sentenced to 25 years to life in a state facility here in California; and 16 years later the same judge that sentenced me to 25 to life re-sentenced me to three years. And I was released that day, which was last year in 2019. I ended up serving 16 years, from 18 up until the age of 34. And pre-COVID I want to say that the conditions inside our prisons are atrocious. Brie mentioned it. They are unsanitary, they are overcrowded.
Adnan: And then you add the concept of power and abuse on top of that, so now we’re talking about the realm of mental health, not just physical health. And I think, in my experience, what I’ve learned and what I’ve actually went through was the lack of response, medically or through mental health, from the administration of our prison system. Now for example, if we’re talking about in terms of COVID, if we’re saying that we’re being told by health professionals to, say for example, stay six feet apart, practice physical distancing…
Adnan: By the way, I want to say that social distancing, that was something that I was sentenced to. I was sentenced to 25 years of life to social distance, so social distancing is possible in prison. Physical distancing is impossible in prison. I want to make sure we use terminology correctly. And so, for example, if I’m being told to stay six feet apart and I live on a tier in San Quentin, which is architecturally made three feet wide, it is physically impossible for me to be six feet apart on a tier of 100 people that is built three feet wide. That’s a small example.
Alex: What’s a tier? What is a tier?
Adnan: I’m sorry. A tier is a floor, so imagine walking on a second floor which is one way in and one way out with 100 people that live on this floor, and it is three feet wide.
Alex: You live on a floor that’s three feet wide, or this is like the-?
Adnan: Yes, with 100 other people.
Brie: Well, there are cells. There are cells on the tier, but then the walkway.
Alex: The walkway is three feet wide, got it.
Brie: The walkway outside of the cells is three feet wise, and so when people are moving it’s not possible to physically distance.
Alex: Not possible. And Eric Maserati-E, I’m going to have to say the last name because we have two Erics on here, what was your experience like? And did you ever live in the bunk situation or were you in even closer contact with other folks?
Eric M.: Yeah, so definitely did everything Adnan just said as far as cell living goes. I’ve done both. The way San Quentin is constructed, it’s a total of three… in total four housing units including death row. But you have GP, or general population, which in that houses North black and West black is where the cells are at. Then you have what’s known as H Unit where it’s a dorm. There’s dorm living. It’s literally a 200 man dorm, 100 bunks in total. And like he was saying, it’s literally physically impossible to do physical distancing.
Eric M.: I’ve literally encountered people being so close. The bunks are so close it looked like they’re sleeping in the same bed, no exaggeration. You will wake up and if you don’t construct your own type of divider then you can literally feel the breath of your neighbor breathing on you if they’re facing in your direction. That’s how close in proximity these bunks are lined up. The construction of these buildings, it’s literally impossible to do any type of physical distancing. And the heightened fear of COVID-19 in there, I can only imagine what they’re going through.
Eric M.: I spoke with several people and people in there are scared, like seriously. And another thing that takes place in there you get penalized, if we will, for trying to do the right thing, and that’s like seek medical attention. The main thing that they’re going to do nine times out of 10 is throw you in the hole and give you an ibuprofen and tell you to drink some water. You know what I mean? It’s a bunch of people that’s nervous to even seek the attention that may possibly be needed.
Eric: Well, can you describe that a little bit more? If I’m seeking medical attention, why are they throwing me in the hole? Can you describe that?
Eric M.: To contain you, first and foremost; to take you away and prevent the spread of whatever it is that you’re seeking medical attention from. Something like this, they’re quarantined in buildings. I’ve been in prison during quarantines, and of course not for this. And to prevent a quarantine, which is like the equivalent to a lockdown for a lot of people because you can’t leave, you’re stuck in a cell, whatever privileges that you have, whatever work that you have, whatever escape that you may have from prison outside of that cell completely gets taken away.
Eric M.: What a lot of people will be coming to my frame up to not jeopardize that is just handle it on their own or whatever, like home remedies they have, to try to prevail over any type of sickness or elements.
Adnan: Well, I just want to add that being sent to solitary confinement is a punishment. And our prison system, obviously, are not hospitals therefore they’re not hospitable. And so the immediate response to a medical response is punitive. And so when someone that has some type of a virus and goes to medical for some type of medical attention… And mind you I want to be fair and say this is not for a minor cough or some sniffles. This is like if you have some type of virus that you feel can be a little epidemic inside the facility. You will be thrown into solitary confinement.
Adnan: Now, once you’re in solitary confinement the rules of solitary confinement apply equally to you whether you are there for quarantine purposes or whether you are there for disciplinary purposes; which means that you don’t have access to your property. And what that means is your letters, envelopes, stamps. You don’t have access to a television. You don’t have access to the telephone to call your family. And so sickness has been dealt with punitively. And because of that fear of being sent to solitary confinement, I have personally never checked into medical when I was sick.
Adnan: And one of the worst sicknesses that I’ve had in my entire life, not just in my 16 years of incarceration I’m talking about my entire life, was about four or five years ago in San Quentin. And I do not know until this day what I had contracted, what type of virus hit me, but all I know is that I could not move without turning… If I turned to my right or left, I was experiencing excruciating pain. I didn’t have an appetite, one because… First, I couldn’t swallow or eat anything. But two, it’s because I didn’t trust the food that the prison serves anyways. I don’t trust its nutritional value and just that it would nurse me back to health. That’s the second thing.
Adnan: All I did was, because of my fear of not going to solitary confinement… And maybe I want to add that my privilege of being relatively young and having a relatively decent immune system, I refused to check into medical. And so I laid on my bunk with excruciating pain, three to four days, barely ate. All I did was drink water from my cell coming from the sink in a prison that’s been around since 1852, by the way. It’s been the first prison built in California, then drinking water out of that faucet that probably hasn’t been changed in over 100 years. I chose to do that besides checking into medical, because of the fear of being sent to solitary.
Brie: And I would just underscore here, from the medical perspective, there is a real need to clarify the difference, and what should be the difference, between solitary confinement, quarantine and medical isolation. And our team at Amend, we’ve been hearing this from, really, around the nation where people are sick, or they have been exposed. They’re being either put into medical isolation wings, or quarantine units, where the same situation that would have happened for them if they were put into solitary confinement for punitive reasons is happening because they’re there for medical reasons.
Brie: Instead, we should really be thinking about people who say that they have a symptom and report that symptom. I mean, they’re doing a huge public service to the entire prison system and to all the staff who are there. And so quarantine is a really important and necessary public health intervention, but what we should be thinking about right now is that these quarantine units should have enhanced opportunities for people to have… In Ireland, they’re giving everybody who has symptoms and is being quarantined, they’re giving them a cell phone so that they can call their family and loved ones outside at any time.
Brie: You can give people movies, 24/7 access to a movie, Netflix. You can give somebody as many books as they want, extra access to canteen, commissary. There are ways that we can use quarantine and develop quarantine wings so that they are not experienced as punitive. And that’s a really important thing that I think a lot of prisons and jails around the nation are learning right now. It’s incredibly important, because people will not tell you when they have symptoms if they’re going to be treated like that.
Alex: I just want to get in and then hand it over to Eric Widera. People listening should go listen to Ear Hustle. It’s a great podcast. I listened to an episode where one of the incarcerated prisoners at San Quentin talks about how he volunteered to care for other prisoners who were sick. And that there was one person who was older, seriously ill, who just absolutely refused to get help; refused to get help because of this concern about the punitive nature of asking for help when you’re sick. A terrific podcast produced at San Quentin. I think Maserati-E is on that podcast that just dropped today as well. Eric, right?
Eric M.: Yeah. I’ll be on there today. Absolutely. Some music is getting featured as well as a brief interview.
Alex: Terrific. And now I’m going to hand it over to Eric Widera.
Eric: All right. We’re talking about physical distancing. What about the other things that we’re recommending people do? Wear face masks, hand sanitizers, wash hands, all of those other things that help control pandemics, can they be done in prisons?
Adnan: Well, I think they require soap, right? And hand sanitizers.
Eric: Yeah.
Adnan: And so hands sanitizers have been considered contraband in prison because of fears of people incarcerated drinking alcohol. Because of that, hand sanitizers have been banned. And now I’m hearing that some hand sanitizers are coming back and they’re on a dispenser that are locked away, so that’s some type of improvement. But I will say that everything in prison costs and what I’m afforded or what I’m actually given by the state department is, one, state made. Meaning the prison, somewhere in the prison factory, incarcerated people are making a very generic bar of soap. And every incarcerated person is given that every week.
Adnan: I think when I was in San Quentin every Tuesday I would get one roll of toilet paper for free by the state and I would get one small generic bar of soap from the state. That one generic bar of soap, if I do not have any money, if I work… And, by the way, if I work at a job I was getting paid 8 cents an hour at this job in the kitchen. It was very difficult to buy a $1 bar of soap at the end of the month, because I have to choose between eating a soup or buying a soap. And so that’s very difficult. And that one bar of soap that’s issued to me is for showers, to wash my face, to wash my body, to wash my hands.
Adnan: That’s the problem in our facilities, that we don’t even have enough to do that, enough soap to keep ourselves clean. As far as face masks, people are putting t-shirts around their faces. Some face masks are being made in the prison industry area. I don’t know how effective they are. I’m hearing stories when one of my friends called me and he says that there was a gentleman who wore glasses who did not want to wear a face mask because it would fog up his glasses. Now I know, spending 16 years in prison, that hypervigilance is an extreme form of survival. I have to be constantly vigilant, keep my eyes open, look at people’s hands, look around, because it’s a punitive and a violent environment, or can be.
Adnan: And because his glasses were fogging up, he did not want to wear a mask because he felt like he had to make a decision between COVID-19 or his physical threat from whoever else. Six officers approached him, this is what I’m being told, without best and handcuffed him and took him to the ground to force him to wear a mask. And these are officers who weren’t wearing masks. Now, this is the one anecdote of someone that called me and told me they saw this happening in the building today. When you look at solutions, hey, wear a mask, can’t you just wash your hands, why not use hand sanitizer, those solutions aren’t actually readily available for people without more problems that come out of it.
Eric: And before we come to solutions, I think for a fair amount of people in the U.S. we may not think about it because we view it as not our problem. This is somewhere else. And it’s interesting because you have this population of people that come from all over the place go into this facility, mix around, be in a place where physical distancing and all these other good quarantine habits are not possible, but we forget then they leave also during this time. And then you also have all the staff at these facilities that also go out, not just correctional officers but others. When you think about this, is this just a prison problem or is this a societal problem?
Eric: Brie That is exactly right. I know that Eric and Adnan have a lot to say about this, I’d just add from the medical perspective. I think that there is a tendency to think about prisons and jails like we were thinking about the cruise ship outbreaks, that these are places that are completely somehow separated from society surrounded by the ocean. But-
Eric: Just let them park way outside of the ocean.
Brie: Just let them pack way away and it’s is going to be their problem, and it’ll be somehow contained there. COVID-19, and any other virus, is not going to respect the walls of a prison. And hundreds… I mean, again, 5,000 prisons and jails and other detention facilities across the nation, it’s mind boggling. These are large facilities by and large 4,000, 5,000, 7,000 people. You’ve hundreds of thousands of correctional officers and correctional healthcare staff coming in and out of these facilities every day, multiple times a day, bringing whatever they’ve been exposed to in the community back into the prison or jail; and bringing whatever they’ve been exposed to in the prison or jail back into the community, to their families, to the grocery store, to the parts where they’re walking around.
Brie: And so this is absolutely not a prison problem. This is not a jail problem. This is not a detention facility problem. This is a United States problem. This is a problem that is borne from mass incarceration. This is a problem that is going to now touch every single citizen in the United States as we fail to get control of a pandemic that we could have gotten control of if we had far fewer people who are incarcerated. And I know we’ll get into solutions later, but if we were willing to depopulate at a much greater scale.
Adnan: Yeah. And to add to that, Brie, exactly. If you look at just California’s numbers, there are close to 120,000 people incarcerated in our state prison facilities; and there are 67,000 staff that come in and out of these facilities, essentially every eight hours. Kind of what you said, Brie. And so even if you look at the concept of commute, how far do people live from where they work? And if you look at correctional officers, how far do they live from where they work? In many rural areas, they live relatively closer.
Adnan: But more prisons, they are surrounded by more communities and more people. Within an hour in any direction is where correction officers or staff stay. Again, 120,000, close to, people incarcerated; 67,000 staff that come in and out of these facilities. And mind you, that’s only California and only California prison numbers.
Brie: It is just California, and that’s not even a federal system or the kennels.
Adnan: No. And that’s not even the… Brie, that’s not even the jail. Just in California, add to that number 110 more jail facilities. Right? Which is almost close to 70,000 more people incarcerated in the jail. Because I want people to know there’s a huge difference between state prison and county jail; and then [abused 00:25:41] difference of private prisons and difference of federal prisons and detention facilities. I’m telling you, they’re all over the United States. And those are just California numbers that I’ve mentioned, so there is no way that we are going to flatten any curve if we do not pay attention to our prison and jail population.
Brie: And we’re not even talking about just flattening the curve of infection, although obviously extraordinarily important. But now there’s enormous concern, as there should be, about restarting the economy. Well, if you look at Santa Barbara, that would have been ready to restart their economy in terms of looking at the requirements put forth by the department of public health and governor Newsome around number of new outbreaks or a number of new cases per day or per week.
Brie: They no longer are able to restart their community and open up their economy because they had a huge outbreak in Lompoc, which is a federal facility in the region. And they had 80 new cases in one day. And so then it actually sets them back for opening their local economy. It’s not just health, this is life. These are jobs. This affects all of us profoundly.
Eric: Okay, so I got a question. Is this a problem that we can’t even solve, so we should just raise our hands; or are there solutions here that we could potentially do to help protect not only the community but the people living inside the walls of these jails and prisons?
Alex: And we always talk about PPE and testing. I’m curious what your sense is of what’s going on, whether there’s adequate protective equipment for healthcare workers, whether there’s adequate testing capabilities in jails and prisons right now? Tell me if you have a sense?
Brie: I would really like to just add one thing here before I hear Adnan and Eric’s responses, and I have some ideas as well. But I just want to make sure that it’s really clear that this is a national issue. This is everybody talking about California law, because we happen to be sitting in California, and these guys recently had experienced in California. But, this is a national problem. And so, again, if you were in one prison or in one jail, you’re in one prison or in one jail. And the most crazy part about this is, again, 5,000 prisons and jails around the nation with 5,000 different problems, 5,000 different potential solutions.
Brie: Just to give you a sense of how poor the testing is. We have, I think, the Marshall project which has done a lot of really great work around collecting data on the number of people who are incarcerated who are infected and testing positive, who are sick or dying. They found that over 21,000 people yesterday, I think, had tested positive for COVID-19. 4,000 of those people are just in two prisons in Ohio that decided to do mass testing. We do not have testing happening, so we don’t even know the scale of this problem. All we know is that when we see it somewhere, especially in one of the dorm settings that Eric described earlier, it’s everywhere.
Brie: But the capacity of prison systems to get the swabs, to get the testing… And then for some prisons, although some systems are being very transparent about their numbers, others are not… and so there are times when people are being tested and we don’t even know what the results are. Although that is not the case in California. And so just to say that the testing… I mean, yes, call for testing, call for testing, but it is not happening. We don’t even know the scope of the problem right now.
Adnan: And to add to that, to make matters more complex, now we’re talking about another type of testing. It was the antibody testing. And today an article came out in New York. They did some antibody testing in some of the state facilities and they were shocked, and it shouldn’t be a shocking reveal, that there are correctional officers who tested for antibodies. And it’s still inconclusive and we don’t know that people who got tested for antibodies can’t get it again. We don’t know that.
Adnan: Yes, I’m not in the medical field but from little that I know there hasn’t been enough information or enough tests being done saying that people who have tested for antibodies cannot get it again. That means there are people walking around who are in our communities, in our prison systems, who still have it and who can still spread it. We’re talking about one wave, now we’re talking about second wave. This is a big problem that’s waiting to happen. When you talk about a big problem that’s not waiting to happen, a big problem that’s going to continue to plague us in society.
Adnan: When we talk about solutions, I think the best solution has to be to decarcerate; that we have to reduce the prison population. There are a lot of people in prison… And we have to do it safely. I’m not asking to let 2.3 million people out of our facilities right now. That’s not practical. But what I’m saying is that it is very easily done. It’s easily done to release people and reduce the prison population drastically. Right now in California alone, we’re like at 120% capacity. Even when something’s 100% full, that’s too much, right?
Adnan: We need to reduce the population so we can make space within our facility so people can try their best to practice physical distancing and try to contain this virus. That’s one thing. But I think what’s happening is… Not I think, but what I truly believe is happening is that it is politics involved, not people. It’s not public health. Because if we were thinking about public health to… decarceration… if we do not reduce the prison population that is a threat to public safety. Politics over people is what’s happening, not people over politics. It took one judge, the same judge who sentenced me to 25 years of life, to say one day, “You know what? I’m releasing you today. I’m not putting you on parole or probation.”
Adnan: It was just the power of one judge that told me I’m safe for society. And it wasn’t politics involved in there. I want to add that. But I do want to… I have a couple of things to say, but I want Eric or Maserati-E to jump in here because I don’t want to take over my… I have a lot of thoughts, that’s why I’m kind of flustered right now on that.
Eric M.: I definitely will piggyback on what you just said. I definitely think, as far as my opinion on it, you hit it dead on the nose. I think decarceration definitely is the go-to route for sure. Based on out in society and the ‘free society’ we’re being encouraged to do physical distancing, we’re being encouraged to do all these different things that just cannot take place in there. What’s only is going to exacerbate this problem. I think on a more, I guess you could say, tangible level for starters let’s get proper PPE in there.
Eric M.: Again, like Adnan said earlier, you got people making their own masks and doing all these things, and that’s because proper PPE isn’t being provided at a high enough rate for everyone to obtain these types of things. I think for starters, definitely make that more priority. You know what I mean? Make sure they’re getting proper care, make sure we’re getting the proper tests, make sure we’re getting proper treatment at the end of the day. And that’s something that I feel the medical field in prisons, at least in my experience in the prisons I’ve been to, continuously neglect the incarcerated population.
Brie: Brie I think it’s really important here to chime in and to say that one way to disrupt this problem around politics over people is to get our messaging straight. This is about depopulation and decarceration, and as ridiculous as it may seem it’s not necessarily around release. For example, if public health is first and if public health is the goal and we really want to keep our communities, our staff, and the people who are incarcerated and everybody who interacts with them safe, then we would have fewer people inside. But there are a lot of different ways to achieve that.
Brie: And depending on the state, and depending on the county, and depending on the jurisdiction there are different things that you can pull on. And so, for example, many people can be released. Many people can be released early. Many people are going to be released in two months, so today would be a better day than in two months. Some people are going to be released in a year, so today would be a better time than in a year. Some people can go home or go to their mother’s house, or their brother or sister’s house, with an ankle bracelet and finish up their sentence there. They don’t have to have their sentence changed.
Brie: They can finish their sentence just in an alternate way, a way that is more in line with public health. Some people are waiting for compassionate release who are seriously ill or dying. There’s 177,000 Americans who are over the age of 55 who are incarcerated in U.S. prisons and jails. And so those people who are waiting for a judge to decide on compassionate release because they have serious illness, they’ve been found to have a terminal illness anyway aside from COVID and now they’re just waiting for the administrative program to wind its way through the course, those are people who are already determined by a physician to be in very, very poor shape.
Brie: And so if they get COVID, that’s kind of it. But there are also furlough programs that we don’t use the United States anymore, that were one time made for like if your daughter is getting married or if your mother dies to go to the funeral or to see that somebody on their death bed outside for an hour or two hours. We could be using furloughs and have people go out. And people who have been determined not to be an immediate threat to society, they could go out and they can come back and serve their time in three years when we have a vaccine.
Brie: We can fight later about whether or not they should come back. We can fight later about mass incarceration and what we’re doing in terms of having so many people incarcerated. But right now I think it’s very important to get the language straight, that what we’re talking about is public health focused decarceration and depopulation. And we can fight later about what that means in terms of sentences, we just need to get people out of overcrowded facilities so that we can bend the epidemic curve.
Eric: Can I ask about that? If the focus is on getting people out, and I’d love to hear both Eric and Adnan’s experience of what was it like to leave, but I’m guessing… And, again, I don’t know but I’m guessing our society does not, “Hey, you’ve served your time. Here are a bunch of resources to make sure you’re landing on your feet when you leave this prison. Here’s a place you can go to you if you were formerly homeless or now homeless, because you don’t have a place to go to.” What does getting out look like for these people, if they get an early release?
Adnan: Well, I’ve been saying for a while now that as we think about reducing the prison population we should equally be thinking about safe housing and proper financial aid. Because not only are we asking for the reduction of the prison population and having people come back into our communities in the middle of a pandemic, but they’re also coming back in the midst of an economic crisis. And so I think that it’s very, very important as we talk about reducing the population to think about safe places where people can be housed, if it is their own homes, if it is other shelters. And be a little more creative.
Adnan: Our organization is reaching out to unused churches, mosques, synagogues, to convert some of those locations for some beds and some housing. And just be creative in that type of space. The other thing is proper financial aid. People are not going to come out and immediately get a job, but there is government assistance. There are ways where people can… whether it’s coming from private donors or whether it’s coming from the government themselves, to give people some type of financial aid. It’s very, very possible.
Adnan: And I also want to think about as we talk about reducing the population, we constantly look at the front door of prisons but not the backdoor of prisons. And so when we talk about this idea of safety, actually factually the safest population to release… factually the safest population are the people who have spent lengthy time or have been sentenced… one, sentenced to life in prison who has spend decades or so in prison. They have less than 1% recidivism rate. And that 1% isn’t from new crimes, it’s something like not going to your transitional home at 10 O’clock instead of coming to your transitional home at 10:30 and you’ve violated parole.
Adnan: Those are the types of things that the less than 1% have been violated for. I want to introduce a mentor. I’m not going to say his name, but he’s 68 years old and he’s been in prison for 42 years. He’s 68 years old, been in prison 42 years, hasn’t had a disciplinary infraction in over 30 years; and so there is no way people can say that he is not safe for society. And so, again, it goes to politics over people and we focus on people’s crimes and not who people are today. Alex and Eric, ask yourselves are you the same person you were 15 years ago, 20 years ago? Are you the same person you were five years ago?
Brie: That’s right.
Adnan: And people change. People, factually, age out of crime. We know that crime, or acts of violence, or a criminal act is very impulsive. And so it has to do with a lot of emotional trauma, lack of emotional responses from community, from society, with healthcare, education. All of those things are actually drivers of incarceration. When you look at incarceration, it’s actually a symptom of a failed government. And we constantly blame people that, “You’re dangerous. You’re dangerous. We’re not letting you out, because you’re dangerous and you’re going to come out and harm us.” And that’s actually not true.
Adnan: If you just look at numbers and you follow the data, that’s actually not true. I want us to think about, as we do reduce the prison population, who are we talking about? All right? Are we just talking about people who are from the front door or are we talking about people who are a certain age group; and how are we defining safety? And how are we defining what’s considered violent people? Because I was considered a violent person until literally the moment the judge says, “You’re walking out the door.”
Alex: That’s terrific. It’s a terrific testament. I want to open the door here to Eric Maserati-E and Brie, to see if there are other ideas that you have. We’ve talked about a number of issues including testing, PPE. We’ve talked about decarceration. What else can we do? And what could our listeners do, who are primarily clinicians, primarily caring for older adults or people with serious illness? Is there one or two things you would ask of them to do at this time?
Eric M.: I think for starters, just awareness is one of the biggest things. I feel like you can’t combat what you don’t know exists. I think a lot of people aren’t even having prisons on their radar as far as this being a problem, especially a potential fact that can exacerbate this pandemic if we will. Right? I think that perception and perspective alone can begin to make a difference. Because, again, you can’t combat what you don’t know exists. That allows the higher ups, if we will, to get away with a lot. What people don’t know is necessarily a problem can allow a group of people to oppress another, if we will.
Eric M.: I think we’ve seen it plenty of times within the civil rights movement what that awareness alone can do, and the type of change that can bring, and what that can spark. That’s one thing I would encourage the people to do. It’s definitely spread the word on that and look into these type of things, understanding and [inaudible 00:40:54] how it can affect them.
Alex: That’s terrific. Brie or Adnan?
Brie: I would echo a lot of what Eric and Adnan have said. I think that, for your listeners, there’s two questions. What can I do as a citizen? And what can I do potentially as a healthcare professional? If that’s what your listeners are mostly. I’d say another thing that as a citizen we can do is give political cover to our politicians that decarceration is acceptable right now; that we understand that controlling this pandemic is going to require that we empty people from prisons and jails, that we understand that important financial resources are going to have to go into resettling them into our communities in a safe way.
Brie: And that we are going to give politicians the political cover to make those hard decisions, and that it is not business as usual right now. I think that that is incredibly important for our entire society to really say on this. In terms of what can healthcare professionals do, I do want to bring up one thing that has been extraordinarily concerning for our team and really just deeply troubling on a personal level as a palliative care doctor and geriatrician; which is that we’re now starting to get phone calls from community physicians and community ethics boards from community hospitals that are for the first time ever taking care of not one person who’s been incarcerated and sent to their hospital facility but six or 10 or 20, or in one case 40.
Brie: These are often very small community hospitals. They have just a few ICU beds, and suddenly those ICU beds are filled with patients who have come from a prison and the doctors and other healthcare professionals have not necessarily taken care of a patient who’s incarcerated. And there’s a lot of confusion about dying patient’s rights. And I just want to remind your listeners, because I think that this is going to become more and more common if we don’t get a handle on this and prisons and jails. I just don’t see how there’s any escaping this situation. That there are three things I want to remind people are really critical for everybody at the end of life, including people who are incarcerated.
Brie: And as number one, people who are incarcerated can make an advanced care plan and they can change their advanced care plan. And one of the big problems that we’ve been hearing recently is perhaps there’s miscommunication between the prison and the hospital. Sometimes it’s one problem, sometimes it’s a different problem. But what ends up happening is there’s miscommunication and misunderstanding that it’s not just that a person who’s incarcerated can make a choice about do not resuscitate and CPR and things like that. But they can make decisions about dialysis and aggressive life sustaining care versus a focus on palliative care and intensive palliative care interventions.
Brie: They can elect somebody to be their durable power of healthcare attorney, or a surrogate decision maker, in the event that they cannot make a decision for themselves. And that doesn’t mean just that the warden calls up the family member, which is a case that we heard recently… A warden calls up a family member and says, “Make them DNR. You’re the surrogate decision maker.” And the family didn’t even know they were hospitalized, let alone seriously ill and ventilated. But that, actually, they have a right to talk to the treating physician or other health care professionals, that they have a right to learn what the status is and to make an informed decision that they would make for a patient who is not incarcerated.
Brie: But those are incredibly important rights and an ethical approach to taking care of patients at the end of life, whether or not they’re incarcerated. That remains a right when people are incarcerated. And third, this is a right for federal prisoners under the first step act but it’s not necessarily a right in all states. But it is part of our, I believe, medical code of ethics, which is that everybody has the right to say goodbye. And we are hearing nurses who are being physically restrained from going into community hospital rooms with a padlet for a family member to say goodbye to their loved one who’s being compassionately exacerbated. There are horror stories from a palliative care perspective.
Brie: And I encourage all of our colleagues around the nation to understand what a serious problem this is. And too, I encourage you that when you see care that does not feel right to you, that does not seem like it upholds the ethical standards that we believe that every person has a right to have at the end of life and in serious illness, that you say something and that you find out the facts. Because very often the facts that are being presented to you may not be the actual rights of the person who you’re taking care of.
Eric: I want to thank you, Brie. And I also want to be mindful of all of your time. I’m going to turn to both Adnan and Maserati-E and ask if you have any other final thoughts for our listeners. Adnan, I’ll start with you.
Adnan: I think I just want to leave people by saying that, yes, when I was 18 years old I committed a crime that I took full responsibility and I still take full responsibility and accountability for. What that means for me, and what remorse, and what harming the community means for me is something that I can never articulate to people. It’s something that I live with every day. Because I’m free, it doesn’t mean that I’m free of guilt. I want to tell society that what I did at 18 years old is a struggle that I’ve been living with, and I’m going to live with my entire life.
Adnan: And, having said that, I also want to say that I’m still a human being. I was incarcerated as a brother, as a son, as a nephew, as a cousin; and when I came out I was still all of those things. I want to say that I matter too. I matter to someone. And now we’re understanding that the interconnectedness that we all need to defeat COVID19 is like now I want everyone to know that you matter to me. And I hope that I matter to you. I’m a human being. My mentor that’s 68 old, that’s been incarcerated for 42 years, is a human being. He’s not the same person. He was 42 years ago in 1978.
Adnan: And so I think this is a humanitarian issue and overall, above all; and what it’s going to require is the characteristics and qualities of human beings such as empathy, forgiveness, care, comfort, love. That’s what’s going to defeat COVID19. I want to call that out in every individual, myself included, incarcerated people included, and all the listeners here on this podcast as well.
Eric: Thank you, Adnan.
Eric M.: Definitely. Thank you for that. I definitely agree with that 100%. That’s definitely the route I was going to go with it as well. It’s the saying that I say all the time, people treat you how they see you and that’s lethal when you’re not seen as an equal. I completely agree. I definitely think it’s a humanitarian matter, if we will. Right? I think one of the biggest things that people operate on when it comes to anything that has to deal with people that are currently incarcerated, they operate out of fear.
Eric M.: And that’s due to various things, right? Media, in my opinion, being one of the main ones that control the narrative when it comes to incarcerated people. And that’s why First Watch was so big in my eyes and so powerful, because that was able to give the currently incarcerated individuals an opportunity to tell their own truth straight from the horse’s mouth and show that visually. And, again, I think the power of perception goes so far. Again, people treat you how they see you; and that’s lethal when you’re not seen as an equal.
Eric M.: Once we begin to be seen as equals, once we begin to be seen as that brother, father, son, and things like that, I think the effort to make sure that we receive proper care in various ways will be far greater. I think we’ll see a lot more effort. And I think we’ll begin to see the conditions change because, ultimately, they’re desiring to change. I think that’s what it’s really going to take for sure.
Eric: I want to thank all of you for joining us today.
Alex: Thank you so much.
Eric: Yeah, especially for shining a light on this huge issue.
Brie: Thank you so much for being brave enough to bring this question onto your podcast. We really appreciate it as well. And I also just want to say that now Adnan is also known as a father, so congratulations to you.
Eric: Congratulations.
Alex: That’s right. Thank you for doing this, what? Two weeks in?
Adnan: Yeah, my son is 15 days old.
Alex: Yeah, still counting days.
Eric: Congratulations.
Alex: It’s awesome.
Eric: Well, before we leave I want to hear more of Eric’s songs. Eric, do you have another song that you can show us… sing to us?
Eric M.: Yes, I do. This song is called Break the Mold. It was featured on a Netflix documentary, Kubo. You could check that out. Kubo is on Netflix right now. We just recently got nominated for two Emmys too, so that’s huge right there. Technically, a Emmy nominated artist, which is nuts.
Alex: That’s great.
Eric M.: Yeah. This song, Break the Mold, is just really geared towards, in a nutshell, what I feel would be the power of unity, if we will. If we come together we can change the world forever. And I truly, truly believe that. And I think that is in perfect correlation of exactly what we were just speaking upon right now, how if we were all to come together we would see a huge difference for sure.
Alex: Awesome. Look forward to… Let’s hear it. And again, we’re going to put a link to Eric Maserati-E’s YouTube channel, and I believe there’s a video of you playing Break the Mold. Was that the one in the church?
Eric M.: Yes. That actually was during a performance for Shakespeare. I also was involved with Shakespeare in there. Yeah, so during the Shakespeare play we are afforded the opportunity to do parallel plays where we do an actual Shakespeare play and then whatever was the main theme of that play we create our own plays utilizing the same themes. And I was requested to do that for one of my friend’s parallel plays.
Eric: Love to hear it.
Eric M.: All right, let’s get it. Let’s get it.
Eric M.: (Singing)
Alex: That’s so good. You are such a good performer. And you wrote those lyrics too?
Eric M.: Absolutely. Absolutely.
Alex: And I saw you have a book of like hundreds of songs.
Eric M.: Yes, I got it. I accumulated about 13 composition books, and I have literally over 500 songs. The last time that I counted I was a little bit over 500, at like 512.
Adnan: That you wrote in prison?
Eric M.: That I wrote in prison, yes.
Eric: And that guitar is from prison? You had that guitar set your incarceration?
Eric M.: Absolutely. This Re:store Justice pit, this is from prison.
Brie: Nice.
Eric M.: Except for this one and The Last Mile one are all from prison, no exaggeration.
Brie: You got to have an online concert.
Eric M.: Oh, definitely. That’s definitely coming sooner.
Brie: Let us know. Put us on the list.
Eric M.: Absolutely. Absolutely.
Brie: Thanks Eric.
Eric: Again, we’ll have links to Eric’s YouTube page. We’ll have links to Re:store Justice on our GeriPal website. Really encourage all of our listeners to check those out. A very big thank you to all three of you for joining us today, really truly honored for having you here. And a thank you to Archstone Foundation for your support for putting this together, and all of our listeners for their continued support.
Alex: Thanks folks, till next time.